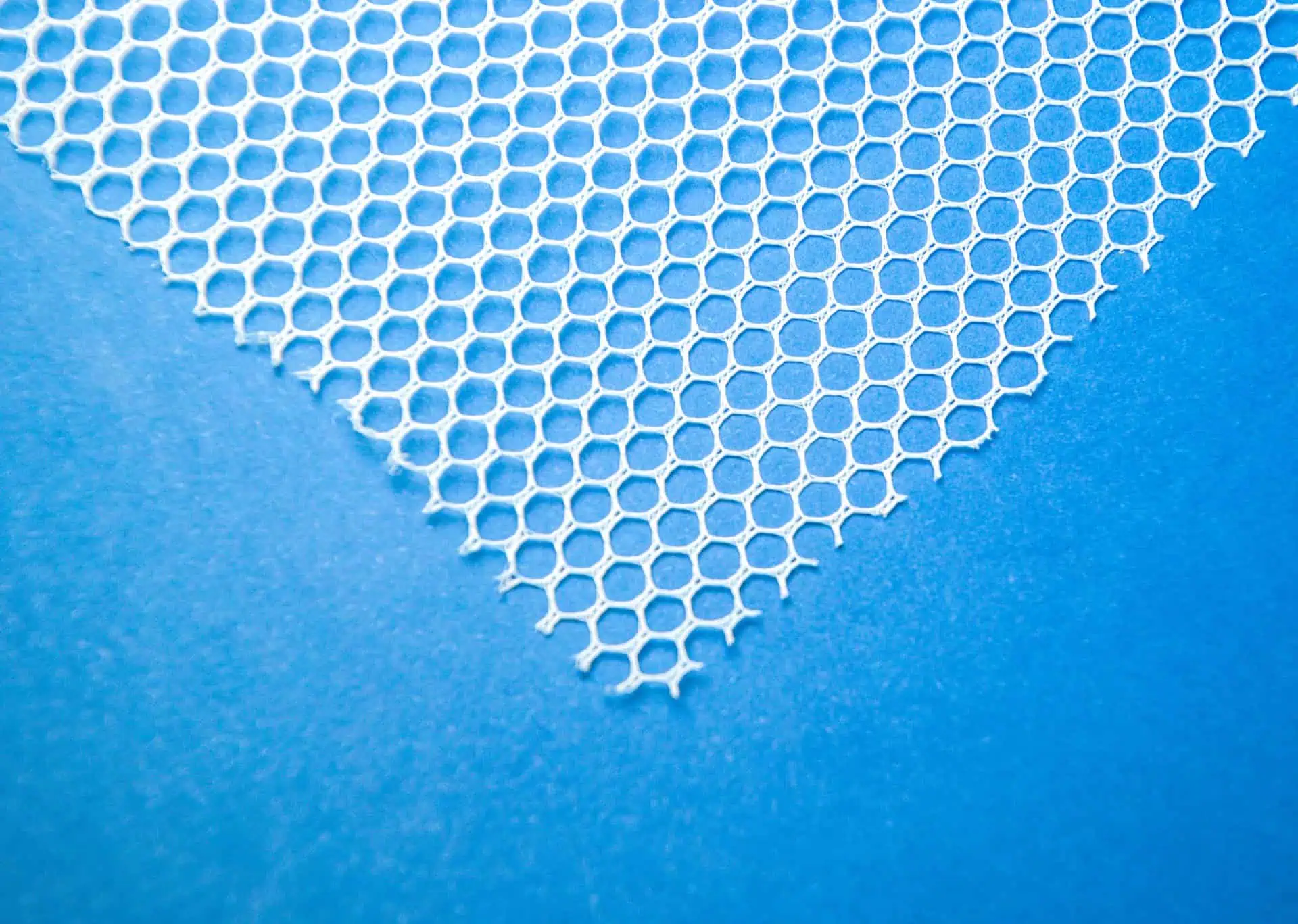
When complications arise from transvaginal mesh, patients face decisions about treatment approaches that balance symptom relief against the potential challenges of additional surgical interventions.
The management of mesh-related issues has developed into a specialized field, with dedicated experts focusing on techniques to address complications while minimizing further harm.
Patients experiencing symptoms have several pathways available, ranging from conservative measures for minor issues to extensive surgical interventions for severe complications.
Treatment Options for Mesh Complications
Managing mesh complications requires individualized care that considers the specific complication type, its severity, the patient’s overall health, and their personal preferences.
The treatment options may range from non-surgical choices to various levels of surgical intervention depending on the clinical presentation.
For minor mesh exposure without symptoms, conservative management may be appropriate.
This option might include topical estrogen therapy to improve vaginal tissue health and potentially assist with covering small areas of exposed mesh.
Close monitoring ensures that the exposure doesn’t worsen over time.
Some patients with mild, tolerable symptoms may choose watchful waiting, particularly if they have medical conditions that increase surgical risks.
The treatment options to address your transvaginal mesh complications include, but are not limited to:
- Partial mesh excision: Removal of only the problematic mesh portion, leaving well-incorporated sections intact. This targeted option may be suitable for localized exposure or erosion when the remainder of the mesh is functioning properly without causing symptoms.
- Complete mesh removal: Excision of the entire mesh implant, which may be necessary for widespread complications, infection, or severe pain syndromes. This procedure often requires extensive dissection and careful identification of mesh arms and anchoring points.
- Staged procedures: Sometimes complete removal is performed in multiple surgeries to reduce operative time and blood loss, particularly for cases involving multiple mesh placements or extensive scarring.
Surgical options may be transvaginal, abdominal (open or laparoscopic/robotic), or a combination depending on the location of the mesh and extent of the complication.
Each option carries different risks and benefits.
The transvaginal route offers direct access to exposed mesh in the vagina, while abdominal options may be necessary to access mesh components near the bladder, bowel, or pelvic sidewall.
Outcome studies show that pain symptoms improve in 60-80% of patients following mesh removal surgery, though complete pain resolution is not guaranteed.
The success rate for resolving mesh erosion is higher, with most patients experiencing resolution after proper excision of the exposed material.
Mesh-Free Options for Pelvic Reconstruction
For patients who require pelvic floor support after mesh removal or those seeking alternatives to mesh for initial treatment, several effective mesh-free approaches exist.
These native tissue repairs use the patient’s own tissues to restore pelvic support without introducing synthetic materials.
Native tissue repairs have experienced renewed interest following concerns about mesh complications.
These techniques have been refined over many decades and offer effective options with potentially fewer long-term complications, though they may have higher anatomical recurrence rates in some studies.
Common native tissue repair approaches include, but are not limited to:
- Anterior and posterior colporrhaphy: Traditional repairs that plicate (fold and suture) the weakened fascial layer of the vagina to reinforce the anterior or posterior compartments.
- Sacrospinous ligament fixation: This technique attaches the vaginal apex to the sacrospinous ligament to provide apical support, especially important after hysterectomy to prevent vaginal vault prolapse.
- Uterosacral ligament suspension: Provides apical support by attaching the vaginal apex to the uterosacral ligaments, which normally support the cervix and upper vagina.
- Iliococcygeus fascia fixation: An alternative apical suspension technique that may be used when the sacrospinous or uterosacral ligaments are unsuitable.
- Fascia lata slings: Uses the patient’s own harvested fascia as material for slings or support, reducing the risk of foreign body reactions but requiring an additional surgical site.
Some surgeons also utilize biologic grafts derived from human or animal tissues as an intermediate option between synthetic mesh and native tissue.
These materials may provide additional support while potentially avoiding some mesh-related complications, though they typically break down over time.
The selection of the appropriate native tissue technique depends on the specific anatomical defect, the patient’s overall health and tissue quality, prior surgeries, and surgeon expertise.
For patients with recurrent prolapse after failed native tissue repair, these procedures can often be repeated or combined with different approaches to address specific weaknesses.