FAQ: What is Trans Vaginal Mesh Used For?
- Last Updated: July 14th, 2025

Attorney Jessica Paluch-Hoerman, founder of TruLaw, has over 28 years of experience as a personal injury and mass tort attorney, and previously worked as an international tax attorney at Deloitte. Jessie collaborates with attorneys nationwide — enabling her to share reliable, up-to-date legal information with our readers.
Legally Reviewed
This article has been written and reviewed for legal accuracy and clarity by the team of writers and legal experts at TruLaw and is as accurate as possible. This content should not be taken as legal advice from an attorney. If you would like to learn more about our owner and experienced injury lawyer, Jessie Paluch, you can do so here.
Fact-Checked
TruLaw does everything possible to make sure the information in this article is up to date and accurate. If you need specific legal advice about your case, contact us by using the chat on the bottom of this page. This article should not be taken as advice from an attorney.
Key takeaways:
- Transvaginal mesh is a device used to support weak pelvic organs in women, often applied for conditions like stress urinary incontinence and pelvic organ prolapse.
- The mesh comes in different types such as non - absorbable synthetic, absorbable synthetic, biological and composite meshes.
- Complications from using transvaginal mesh may include pain during intercourse, severe infections, persistent vaginal bleeding or recurrent urinary tract infections.
- Before opting for a treatment involving transvaginal mesh, it's crucial to have an informed discussion with your doctor about potential risks and alternatives.
What is Trans Vaginal Mesh Used For? Let's Discuss.
Question: What is Trans Vaginal Mesh Used For?
Answer: Trans vaginal mesh is a synthetic net-like substance used to provide extra support for repairing weakened or damaged internal tissue in the pelvic area. The mesh is implanted through a small incision in the vaginal wall to reinforce the weakened tissue and provide structural support.
Transvaginal mesh is used for the following purposes:
- Treatment of Pelvic Organ Prolapse (POP): Transvaginal mesh is used to repair weakened or damaged tissue in the pelvic area, specifically to support prolapsed organs. In this surgery, an incision is made in the vaginal wall, and the mesh is inserted to help hold up the fallen organs.
- Treatment of Stress Urinary Incontinence (SUI): Transvaginal mesh can also be used to support the urethra or bladder neck for the repair of stress urinary incontinence. It provides additional support to prevent urine leakage during physical activities that put pressure on the bladder.
- Reinforcement of the Vaginal Wall: Transvaginal mesh is permanently implanted to reinforce the weakened vaginal wall for pelvic organ prolapse repair or support the urethra or bladder neck for stress urinary incontinence repair.
On this page, we’ll provide an in depth answer to “what is Trans Vaginal Mesh used for?”, discuss potential complications with Transvaginal Mesh Implants, review alternative treatment options to Transvaginal Mesh, cover the Transvaginal Mesh Lawsuits, and much more.

While transvaginal mesh has been effective for many patients, there have been reports of complications associated with its use.
These complications can include pain, infection, erosion of the mesh into surrounding tissues, and recurrence of the original condition.
Overview of Trans Vaginal Mesh Usage
In recent years, there has been increased scrutiny and legal action related to the safety and effectiveness of transvaginal mesh implants.
In response to the reported complications, regulatory agencies such as the U.S. Food and Drug Administration (FDA) have taken action to address the safety concerns associated with transvaginal mesh.
In some cases, specific types of mesh have been banned or restricted for use in certain procedures.
Table of Contents
What is Transvaginal Mesh?
Transvaginal mesh is a medical device, typically made from synthetic materials or biological tissue, designed to provide support for weakened pelvic organs in women.
Its main purpose is to assist with conditions such as pelvic organ prolapse (POP) and stress urinary incontinence (SUI).

This mesh comes in several types, each specifically addressing different needs and procedures.
Several manufacturers produce these meshes under various brand names.
Organ Prolapse and Stress
Transvaginal mesh functions as a net-like implant used in surgical procedures. This medical device works to repair weakened or damaged tissue in the pelvic area or bladder of a woman.
The design offers additional support to treat pelvic organ prolapse as well as conditions such as stress urinary incontinence. Despite recent FDA restrictions, transvaginal mesh still plays an essential role in many pelvic surgeries not associated with prolapse repairs.
Prolapse and Stress urinary incontinence
Transvaginal mesh serves a critical role in women’s health, primarily dealing with stress urinary incontinence and pelvic organ prolapse.
These conditions often occur after childbirth, menopause, or a hysterectomy and can cause discomfort or even pain in daily life.
Women who struggle with the burdens of these medical circumstances find relief through the use of transvaginal mesh.
The primary objective of this surgical procedure is to provide support to weakened pelvic organs.
The versatility of transvaginal mesh allows physicians to employ it individually or combine it with other surgical procedures treating urinary incontinence.
This supportive device qualifies as safe by FDA standards; thus ensuring its solid positioning and anchoring without inducing significant complications.
Types of Transvaginal Mesh
Understanding the varieties of transvaginal mesh is essential for making informed healthcare choices.
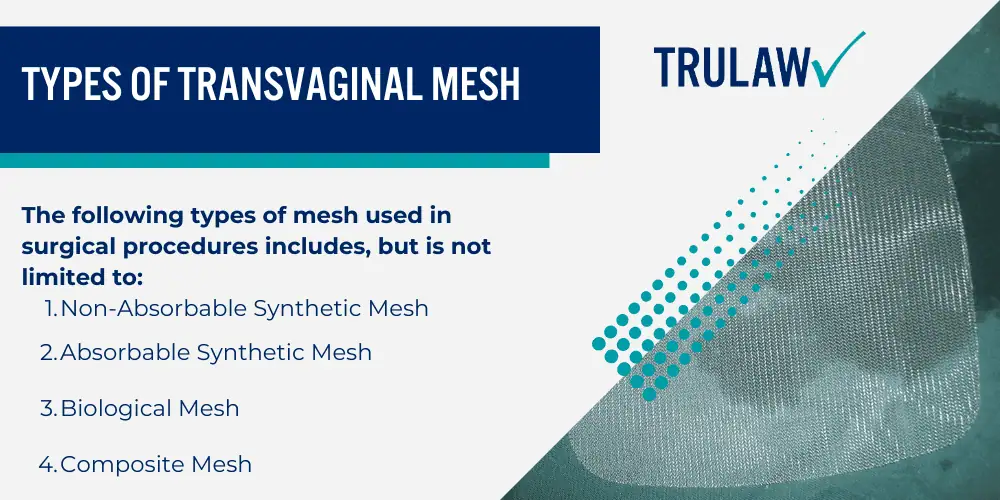
The following types of mesh used in surgical procedures includes, but is not limited to:
- Non-Absorbable Synthetic Mesh: This type is made from synthetic materials that permanently stay in the body, providing long-term support to weakened tissues.
- Absorbable Synthetic Mesh: Over time, your body gradually absorbs this synthetic mesh. It temporarily supports damaged tissues as they heal.
- Biological Mesh: Derived from animal tissue, usually pig or cow, that’s been disinfected for safe medical use. This organic mesh also gets absorbed by your body over time.
- Composite Mesh: A combination type using different materials like synthetic and biological components.
Manufacturers and Brands
Numerous companies manufacture transvaginal mesh, contributing to a vast range of brands and products.

While this list isn’t exhaustive, it provides an idea of the diversity in the market:
- Boston Scientific
- Johnson & Johnson
- Bard Medical Division
- Coloplast Corp.
- American Medical Systems
Transvaginal Mesh Usage and Treatment
Transvaginal mesh is primarily used as a treatment for two conditions – pelvic organ prolapse and stress urinary incontinence, proving to be an effective but debated method.

Dive deeper into the specifics of when transvaginal mesh becomes necessary by continuing on with our comprehensive guide.
Treatment for Stress Urinary Incontinence
Stress urinary incontinence can be effectively treated using transvaginal mesh.
This medical device has a strong success record for patients who have not benefited from non-surgical treatments.
One of the most common procedures is the midurethral sling, which helps control leakage by supporting the urethra.
Transvaginal mesh implants are beneficial for incontinence treatment despite facing an FDA ban on their use for prolapse repairs due to potential complications.
The Food and Drug Administration continues to monitor any serious issues arising from most surgical mesh implants.
So far, its usage remains effective for stress urinary incontinence treatment.
Alternative Non-Surgical Treatments
Before considering transvaginal mesh as a treatment for pelvic floor disorders, it’s important to discuss alternative non-surgical treatments with your doctor.
These options may pose less risk and can be quite effective:
- Physical Therapy: This option focuses on exercises that strengthen the pelvic floor muscles.
- Lifestyle Modifications: Changes in your diet, fluid intake, and weight loss can significantly improve symptoms.
- Use of Pessaries: Pessaries are devices inserted into the vagina to support structures such as the uterus or bladder.
Potential Complications with Transvaginal Mesh Implants
Mesh erosion is one of the major complications that may arise with transvaginal mesh implants, causing pelvic pain and potential damage to surrounding organs.
This problem often requires additional surgeries to fix, which can lead to further health risks.
Pain during sexual intercourse is another commonly reported issue, caused by the exposure of the mesh into the vagina.
Complications do not end there; they may also include severe infections leading to persistent vaginal bleeding or discharge.

Recurrent urinary tract infections (UTIs) are a common aftermath of transvaginal mesh implantation as well.
These UTIs often require rigorous treatment and can drastically affect a woman’s daily life activities.
It’s crucial for any woman considering this procedure to understand these potential complications before making an informed decision on their health care choice.
Are You Experiencing Pain or Discomfort After Transvaginal Mesh Implantation?
Pain or discomfort can be a sign of complications after transvaginal mesh implantation.
These problems might include infection, bleeding, and even the erosion of vaginal tissue.
It’s also worth noting that not every woman who experiences pain has these severe complications.
Many women experience mild discomfort that improves over time as the body heals from surgery.

In some cases, however, post-implantation pain could be indicative of a more serious issue such as mesh shrinkage or contraction which may pose long-term health risks.
Some patients report persistent pelvic or abdominal pain and others notice increased urinary frequency or urgency.
The exact causes of this chronic pain following transvaginal mesh surgery are currently under investigation to improve patient outcomes and reduce any associated suffering.
Seeking Medical Advice
If you’re noticing any discomfort from your transvaginal mesh implant, it’s vital to seek prompt medical attention to understand possible treatment options and navigate through potential complications.

Importance of Seeking Medical Attention
Proactively seeking medical attention is vital, particularly when considering the use of transvaginal mesh.
This step can help mitigate potential complications and ensure your overall well-being.
Medical professionals offer valuable guidance based on their vast knowledge and experience in dealing with such cases.
The FDA safety communications emphasize the significance of informed healthcare decisions about devices like transvaginal mesh.
With their help, you can gain a clear understanding of all aspects involved – from the procedure itself to possible risks and complications.
Hence, it’s essential not just for treatment but also for preventing any harm to your health.
Possible Treatment Options
Medical professionals consider several treatment options for pelvic floor disorders.
Patients can explore the following choices depending on their specific condition and medical history:
- Non-surgical treatments: These encompass pelvic floor therapy, biofeedback, and pessary use. In some cases, lifestyle changes such as weight loss or cessation of smoking can make a significant difference.
- Medications: Certain drugs are effective in managing symptoms of stress urinary incontinence and pelvic organ prolapse.
- Native tissue repairs: This surgical treatment option uses the patient’s own tissues to repair the prolapsed area.
- Transvaginal mesh implantation: Physicians resort to this solution when other treatments have failed. However, due to multiple reported complications, the FDA has banned transvaginal mesh for treating pelvic organ prolapse.
- Laparoscopic sacrocolpopexy: This is a minimally invasive procedure that uses a synthetic mesh to hold the vagina in its normal position but through an abdominal approach rather than transvaginally.
- Sacrospinous ligament fixation: Surgeons use stitches to attach the vaginal wall or cervix to the strong sacrospinous ligament on one side of the pelvis correcting vaginal prolapse.
Support Services Available
Various support services exist for individuals who have had transvaginal mesh implants, including the Victorian Mesh Information and Helpline, peer support groups, hospital programs, and additional resources to provide comfort and assistance during this time.

Victorian Mesh Information and Helpline
The Victorian Mesh Information and Helpline stands as a valuable resource for women needing crucial information about transvaginal mesh.
Offering comprehensive support services, this helpline guides individuals who are contemplating this form of treatment or those coping with post-implantation complications.
Besides dispensing critical information, the Victorian Mesh Information and Helpline connects callers to peer-support groups designed to provide emotional comfort and practical advice from those sharing similar experiences.
Hospital programs that specialize in managing conditions such as pelvic or groin pain, and pelvic floor disorder also cooperate closely with the helpline, ensuring callers receive well-rounded guidance.
Peer Support
Peer support holds a substantial role in helping women navigate their experiences with transvaginal mesh.
Participating in peer support groups provides an opportunity for individuals to share personal experiences and feelings, learn effective coping strategies, and gain a sense of empowerment.
These groups also offer chances to connect with others who have been through similar situations, fostering an environment where mutual understanding is deepened.
Personal growth can be achieved by both receiving and offering assistance within these supportive networks.
Volunteers often lead discussions, encouraging open conversation about fears, challenges, and positive aspects of the recovery process.
Hospital Programs
Hospital programs offer an array of services to women dealing with transvaginal mesh complications, such as:
- Specialized assistance: Hospitals have developed programs specifically for women experiencing issues from transvaginal mesh. The focus is on providing support and assistance in managing the complexities associated with this medical device.
- Quality of life improvement: The ultimate goal of these hospital programs is to enhance the quality of life for women affected by transvaginal mesh complications.
- Range of treatment options: Hospitals don’t just provide one solution; they offer a variety of surgical and non-surgical treatments to address difficulties related to transvaginal mesh.
- Comprehensive care: These specialized hospital programs intend to deliver comprehensive care and support for female patients experiencing transvaginal mesh complications, covering all aspects of their health needs.
- Multidisciplinary team: To ensure patients receive well-rounded treatment, hospital programs may include a multidisciplinary team of healthcare professionals such as urologists, gynecologists, physical therapists, and counselors. They collaboratively work together to meet the unique requirements and wellbeing goals of each patient.
Other Materials for Support
Finding the right support after transvaginal mesh implantation is crucial for your recovery process.
Here are some resources you can turn to for help with your vaginal mesh implants:
- In-person and online support groups: These provide a safe space to share experiences, gain emotional support, and learn from others who have gone through similar situations.
- Medical websites and blogs: Websites like WebMD, Mayo Clinic, and Healthline offer valuable information about transvaginal mesh complications and possible treatment methods.
- Books and articles: Many authors have chronicled their personal journey with transvaginal mesh complications, offering insights into dealing with the issue personally and medically.
- Podcasts and videos: A wide range of multimedia resources is available that deal with medical topics including transvaginal mesh implants.
- Peer counseling programs: Some hospitals offer these programs where women who have had similar procedures provide counsel based on their firsthand experiences.
- Patient advocates: They assist in coordinating care, explain medical procedures, answer questions about insurance, rights as a patient, etc.
Alternative Treatment Options to Transvaginal Mesh
In this section, we’ll explore the different surgical and non-surgical alternatives available to transvaginal mesh, providing a comprehensive overview of each treatment option’s potential effects and success rates.

Non-Surgical Options
You have the power to choose from several non-surgical methods to treat stress incontinence.
It’s important to understand all your options, especially if transvaginal mesh isn’t effective or suitable for you.
Here are some common non-surgical alternatives:
- Lifestyle changes: Include regular exercises, diet modifications, and weight management practices.
- Pelvic floor muscle training: This strengthens the muscles that help control urination.
- Bladder training: Teaches you how to delay urination when feeling an urge to urinate.
- Medication: Certain drugs can calm overactive bladder muscles.
- Electrical stimulation therapy: A small electrical current is used to stimulate and strengthen pelvic muscles.
- Magnetic therapy: Uses magnetic fields to stimulate nerve activity and boost muscle strength.
Surgical Options (Without Mesh)
Understanding the different surgical mesh considerations or mesh related complications equips you for an informed discussion with your doctor.
Here are some of the alternatives:
- Native Tissue Repair: This procedure uses a woman’s own tissues to repair the affected area. It effectively treats pelvic organ prolapse and presents lesser complications than permanent mesh.
- Biological Grafts: Surgeons will use sterilized and processed tissues from human or animal donors as implants during surgery.
- Synthetic Non-mesh Implants: These refer to surgeries using synthetic implants that aren’t mesh, such as urethral bulking injections.
- Laparoscopic Sacrocolpopexy: A minimally invasive surgery that supports the vagina by attaching it to strong tissue alongside the backbone.
- Uterine Suspension Using Sutures: The uterus or upper part of the vagina is sewn back into its normal position.
- Colpocleisis: A procedure for women who no longer wish to have intercourse where part or all of the vaginal canal is closed off to provide support for prolapsed organs.
Transvaginal Mesh Lawsuits
Delve into the details surrounding transvaginal mesh lawsuits, including current litigation trends and steps to pursue legal assistance if you have suffered from a faulty implant.

Information on Current Lawsuits
Numerous transvaginal mesh lawsuits currently flood the court dockets.
These legal challenges stem from serious complications women have experienced due to the device.
It’s estimated that the ongoing legal battles amount to approximately $8 billion in personal injury settlements.
Most cases accuse manufacturers of negligence and design defects, with one notable case against Boston Scientific alleging they used counterfeit resin in their product creation process.
This wave of litigation shows no signs of slowing down as more women come forward seeking compensation for damages caused by these medical devices.
How to Seek Legal Assistance
Securing the right legal assistance is crucial when dealing with transvaginal mesh-related issues.

Here are some steps to follow:
- Seek professional legal help with expertise in transvaginal mesh lawsuits.
- Collect all relevant medical documents such as diagnosis, treatments, procedures, and any complications that were experienced.
- Keep a detailed record of the impact on your daily life caused by the mesh implant.
- Consider compiling any communication logs between you and healthcare providers about the mesh complications.
- Make sure to contact a lawyer who has experience in transvaginal mesh cases.
- Discuss potential legal avenues or options with your chosen attorney.
- Check if there are ongoing lawsuits against the manufacturer of your mesh implant, lawyers should be able to provide this information.
- Ensure you are comfortable with your lawyer as they will represent you throughout the legal process.
Concluding Transvaginal Mesh
In closing, acknowledging the potential risks and complications linked with transvaginal mesh implants is crucial.
An attorney’s advice can be invaluable for those who have suffered from its effects.
TruLaw’s Experience With Transvaginal Mesh Lawsuits
If you’re experiencing complications with your transvaginal mesh implant, don’t suffer in silence.
Let the experienced team at TruLaw provide the guidance and support you need.
Reach out to us today for a free consultation — we’re ready to help you navigate through this challenging time.
Transvaginal Mesh Lawsuit Frequently Asked Questions
-
Question: What is Trans Vaginal Mesh Used For?
Answer: Transvaginal mesh is a synthetic net-like substance used to provide extra support for repairing weakened or damaged internal tissue in the pelvic area.
Transvaginal mesh is used for the following purposes:
- Treatment of Pelvic Organ Prolapse (POP): Transvaginal mesh is used to repair weakened or damaged tissue in the pelvic area, specifically to support prolapsed organs. In this surgery, an incision is made in the vaginal wall, and the mesh is inserted to help hold up the fallen organs.
- Treatment of Stress Urinary Incontinence (SUI): Transvaginal mesh can also be used to support the urethra or bladder neck for the repair of stress urinary incontinence. It provides additional support to prevent urine leakage during physical activities that put pressure on the bladder.
- Reinforcement of the Vaginal Wall: Transvaginal mesh is permanently implanted to reinforce the weakened vaginal wall for pelvic organ prolapse repair or support the urethra or bladder neck for stress urinary incontinence repair.
-
The doctors place the transvaginal mesh through the vagina to support sagging organs, helping alleviate symptoms of pelvic organ prolapse and stress urinary incontinence.
It is intended to provide the following benefits:
- Provides additional support to repair weakened or damaged internal tissue
- Helps alleviate symptoms of pelvic organ prolapse or stress urinary incontinence
- Offers a minimally invasive surgical option for women
-
While there are differing opinions on the safety of transvaginal mesh, it is important to be aware of the potential risks and complications associated with this procedure.
Some of the risks include:
- Mesh erosion: The tissue covering the mesh may wear away, causing the mesh to poke through the vaginal skin.
- Pelvic pain: Some individuals may experience persistent pelvic pain after transvaginal mesh surgery.
- Pain during sex: The presence of transvaginal mesh may cause discomfort or pain during sexual intercourse.
- Infections: In rare cases, transvaginal mesh surgery can lead to infections.
- Mesh contraction: The mesh may contract, causing the tissue around it to tighten, which can lead to strictures.
It is important to discuss these risks with a healthcare provider and weigh them against the potential benefits of transvaginal mesh surgery.
-
If you are experiencing complications from transvaginal mesh, it is important to consult with your healthcare provider.
They will evaluate your specific situation and determine if mesh removal is necessary.
Here are some key points to consider:
- Mesh Removal Surgery: In some cases, surgical removal of the transvaginal mesh may be recommended. This procedure is typically performed by a urogynecologist or a surgeon with expertise in pelvic floor disorders.
- Evaluation of Complications: Before deciding on mesh removal, your healthcare provider will conduct a thorough evaluation of your symptoms and complications.
- Risks and Benefits: Mesh removal surgery carries its own risks, including bleeding, infection, and injury to surrounding organs. Your healthcare provider will weigh the potential benefits of mesh removal against the risks involved, taking into account your individual circumstances.
- Alternative Treatments: In some cases, alternative treatments may be considered instead of mesh removal. These can include conservative management strategies, physical therapy, or other surgical interventions.
- Recovery and Rehabilitation: After mesh removal surgery, a period of recovery and rehabilitation is typically required. This may involve restrictions on physical activity, pain management, and follow-up appointments with your healthcare provider to monitor your progress.
It is important to consult with a healthcare professional who specializes in pelvic floor disorders and has experience with transvaginal mesh complications.
They will be able to provide personalized advice and guidance based on your specific situation.
-
Pelvic Organ Prolapse (POP) is a medical condition where weakened pelvic muscles lead to the descent of pelvic organs.
Pelvic Organ Prolapse, commonly referred to as POP, is a condition that affects the pelvic region:
- POP occurs due to weakened pelvic floor muscles.
- It results in the descent or prolapse of pelvic organs.
- Organs like the uterus or bladder can be affected.
The primary cause of POP is the weakening of the muscles in the pelvic floor, which can happen due to various reasons, including childbirth, aging, or other factors.
When the pelvic floor muscles weaken, they can no longer support the pelvic organs adequately, leading to their descent or prolapse.

Managing Attorney & Owner
With over 25 years of legal experience, Jessica Paluch-Hoerman is an Illinois lawyer, a CPA, and a mother of three. She spent the first decade of her career working as an international tax attorney at Deloitte.
In 2009, Jessie co-founded her own law firm with her husband – which has scaled to over 30 employees since its conception.
In 2016, Jessie founded TruLaw, which allows her to collaborate with attorneys and legal experts across the United States on a daily basis. This hypervaluable network of experts is what enables her to share the most reliable, accurate, and up-to-date legal information with our readers!
Additional Transvaginal Mesh Lawsuit resources on our website:
Here, at TruLaw, we’re committed to helping victims get the justice they deserve.
Alongside our partner law firms, we have successfully collected over $3 Billion in verdicts and settlements on behalf of injured individuals.
Would you like our help?
At TruLaw, we fiercely combat corporations that endanger individuals’ well-being. If you’ve suffered injuries and believe these well-funded entities should be held accountable, we’re here for you.
With TruLaw, you gain access to successful and seasoned lawyers who maximize your chances of success. Our lawyers invest in you—they do not receive a dime until your lawsuit reaches a successful resolution!
AFFF Lawsuit claims are being filed against manufacturers of aqueous film-forming foam (AFFF), commonly used in firefighting.
Claims allege that companies such as 3M, DuPont, and Tyco Fire Products failed to adequately warn users about the potential dangers of AFFF exposure — including increased risks of various cancers and diseases.
Depo Provera Lawsuit claims are being filed by individuals who allege they developed meningioma (a type of brain tumor) after receiving Depo-Provera birth control injections.
A 2024 study found that women using Depo-Provera for at least 1 year are five times more likely to develop meningioma brain tumors compared to those not using the drug.
Suboxone Tooth Decay Lawsuit claims are being filed against Indivior, the manufacturer of Suboxone, a medication used to treat opioid addiction.
Claims allege that Indivior failed to adequately warn users about the potential dangers of severe tooth decay and dental injuries associated with Suboxone’s sublingual film version.
Social Media Harm Lawsuits are being filed against social media companies for allegedly causing mental health issues in children and teens.
Claims allege that companies like Meta, Google, ByteDance, and Snap designed addictive platforms that led to anxiety, depression, and other mental health issues without adequately warning users or parents.
Transvaginal Mesh Lawsuits are being filed against manufacturers of transvaginal mesh products used to treat pelvic organ prolapse (POP) and stress urinary incontinence (SUI).
Claims allege that companies like Ethicon, C.R. Bard, and Boston Scientific failed to adequately warn about potential dangers — including erosion, pain, and infection.
Bair Hugger Warming Blanket Lawsuits involve claims against 3M — alleging their surgical warming blankets caused severe infections and complications (particularly in hip and knee replacement surgeries).
Plaintiffs claim 3M failed to warn about potential risks — despite knowing about increased risk of deep joint infections since 2011.
Baby Formula NEC Lawsuit claims are being filed against manufacturers of cow’s milk-based baby formula products.
Claims allege that companies like Abbott Laboratories (Similac) and Mead Johnson & Company (Enfamil) failed to warn about the increased risk of necrotizing enterocolitis (NEC) in premature infants.
Here, at TruLaw, we’re committed to helping victims get the justice they deserve.
Alongside our partner law firms, we have successfully collected over $3 Billion in verdicts and settlements on behalf of injured individuals.
Would you like our help?