How Can Transvaginal Mesh Complications Impact Quality Of Life?
- Last Updated: July 14th, 2025

Attorney Jessica Paluch-Hoerman, founder of TruLaw, has over 28 years of experience as a personal injury and mass tort attorney, and previously worked as an international tax attorney at Deloitte. Jessie collaborates with attorneys nationwide — enabling her to share reliable, up-to-date legal information with our readers.
Legally Reviewed
This article has been written and reviewed for legal accuracy and clarity by the team of writers and legal experts at TruLaw and is as accurate as possible. This content should not be taken as legal advice from an attorney. If you would like to learn more about our owner and experienced injury lawyer, Jessie Paluch, you can do so here.
Fact-Checked
TruLaw does everything possible to make sure the information in this article is up to date and accurate. If you need specific legal advice about your case, contact us by using the chat on the bottom of this page. This article should not be taken as advice from an attorney.
Key takeaways:
- Transvaginal mesh complications include mesh erosion through vaginal tissue bleeding pain during intercourse urinary problems and persistent pelvic organ prolapse.
- Women experiencing transvaginal mesh complications often report chronic pelvic pain vaginal discharge sexual dysfunction infection and difficulty with bowel or bladder function.
- Following FDA restrictions on transvaginal mesh products alternative treatments include native tissue repair, biological grafts, and pubovaginal slings made from the patient's own tissue.
How Can Transvaginal Mesh Complications Impact Quality Of Life?
Question: How can transvaginal mesh complications impact quality of life?
Answer: Women experiencing painful physical symptoms, requiring revision surgeries, or suffering long-term health issues following transvaginal mesh implantation may qualify for legal compensation through a transvaginal mesh lawsuit.
On this page, we’ll answer this question in further depth, examining the physical impact of transvaginal mesh complications, exploring legal options for those suffering transvaginal mesh failures, and much more.

Physical Symptoms of Mesh Failure After Surgery
Transvaginal mesh surgery treats pelvic organ prolapse and stress urinary incontinence that can lead to serious complications for many patients.
Mesh erosion occurs when the synthetic material cuts through vaginal tissue causing chronic pain, bleeding, infection, and painful intercourse.
Over 100,000 women nationwide have reported serious health conditions, such as urinary problems, recurrent infections, difficulty emptying the bladder, and worsening incontinence issues that severely limit daily activities.
If you or someone you love has experienced vaginal mesh complications following transvaginal mesh surgery, you may qualify to seek compensation.
Contact TruLaw using the chat on this page to receive an instant case evaluation that can determine your eligibility to join others filing a Transvaginal Mesh Lawsuit today.
Table of Contents
How Can A Transvaginal Mesh Attorney from TruLaw Help You?
Our Transvaginal Mesh lawyer at TruLaw is dedicated to supporting clients through the process of filing a Transvaginal Mesh lawsuit.
With extensive experience in product liability cases, Jessica Paluch-Hoerman and our partner law firms work with litigation leaders and medical experts to prove how defective mesh implants caused you harm.

TruLaw focuses on securing compensation for medical expenses, revision surgeries, pain and suffering, lost income, and other damages resulting from your transvaginal mesh injuries.
We understand the physical and emotional toll that Transvaginal Mesh complications have on your life and provide the personalized guidance you need when seeking justice.
Meet the Lead Transvaginal Mesh Attorney at TruLaw
Meet our lead Transvaginal Mesh attorney:
- Jessica Paluch-Hoerman: As founder and managing attorney of TruLaw, Jessica brings her experience in product liability and personal injury to her client-centered approach by prioritizing open communication and personalized attention with her clients. Through TruLaw and partner law firms, Jessica has helped collect over $3 billion on behalf of injured individuals across all 50 states through verdicts and negotiated settlements.
How much does hiring a Transvaginal Mesh lawyer from TruLaw cost?
At TruLaw, we believe financial concerns should never stand in the way of justice.
That’s why we operate on a contingency fee basis—with this approach, you only pay legal fees after you’ve been awarded compensation for your injuries.
If you or a loved one experienced pain, bleeding, infection, organ perforation, mesh erosion, or other complications from transvaginal mesh implants, you may be eligible to seek compensation.
Contact TruLaw using the chat on this page to receive an instant case evaluation and determine whether you qualify to join others in filing a Transvaginal Mesh lawsuit today.
Common Transvaginal Mesh Complications After Surgery
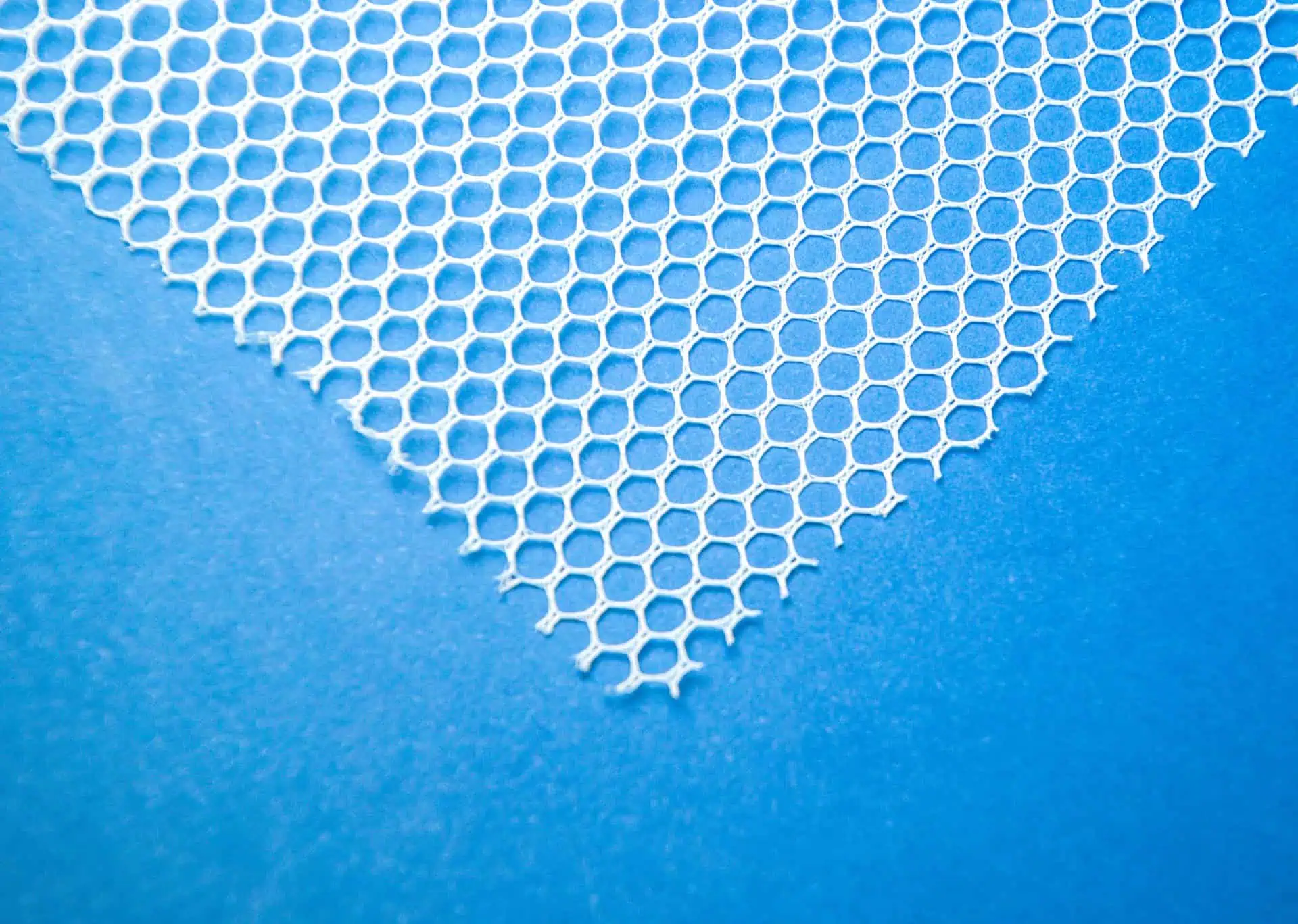
Transvaginal mesh complications represent some of the most serious adverse effects experienced by women who have undergone surgical procedures to treat pelvic floor disorders.

These complications have been extensively documented by the FDA and medical researchers, prompting regulatory actions including reclassification of transvaginal mesh as a high-risk device and eventually banning its use for pelvic organ prolapse repairs due to safety concerns that outweigh potential benefits according to studies from the Mayo Clinic and adverse event data collected by regulatory agencies.
Recognizing Mesh Erosion and Its Physical Symptoms
Mesh erosion, also referred to as exposure, extrusion, or protrusion, occurs when the synthetic material wears through vaginal tissue and becomes exposed.
This process develops gradually as the body’s response to the foreign material causes the mesh to migrate through tissue layers, creating a pathway for infection and persistent tissue damage.
The Food and Drug Administration has identified mesh erosion as the most commonly reported complication of transvaginal POP repair with surgical mesh.

Complications reported by women shortly after undergoing a transvaginal mesh procedure typically include, but are not limited to:
- Physical indicators of mesh erosion include vaginal bleeding or spotting unrelated to menstruation
- Abnormal vaginal discharge, often accompanied by foul odor indicating infection
- Recurrent urinary tract infections resistant to antibiotic treatment
- Palpable mesh fibers that the patient or partner may feel during intercourse
- Severe pelvic or vaginal pain that worsens during specific movements or activities
- Other severe health conditions and injuries
Pain and Discomfort: Ongoing Mesh-Related Complications
Women experiencing transvaginal mesh complications often report debilitating chronic pain as their most significant symptom, dramatically reducing quality of life and necessitating additional interventions.
According to the American College of Obstetricians and Gynecologists, Pelvic pain (including dyspareunia), possibly related to nonexposed mesh may not respond to mesh removal and should prompt referral to a clinician with appropriate training and experience.
This acknowledgment reflects the challenging nature of treating mesh-related pain syndromes.
The management of chronic pain after mesh implantation presents substantial challenges for medical professionals, often requiring multidisciplinary approaches including physical therapy, pain management specialists, and potential surgery to remove the offending material.
Research published in the International Urogynecology Journal demonstrates that early diagnosis of mesh complications is crucial for successful treatment outcomes, with complications identified within the first year having better resolution rates than those discovered later.
Even with expert intervention, patients may continue to experience pain and related symptoms for years after the initial procedure, highlighting the importance of proper patient selection and informed consent before utilizing mesh-based surgical approaches.
Physical Impact of Transvaginal Mesh Complications
The physical consequences of transvaginal mesh implants can be devastating and far-reaching, often progressing from moderate discomfort to debilitating pain that impairs quality of life.

While originally marketed as a minimally invasive solution for pelvic floor disorders, the implantation of vaginal mesh has resulted in numerous complications for thousands of women, prompting the FDA to issue warnings and eventually ban transvaginal mesh for pelvic organ prolapse repair in 2019 after determining that the risks outweighed potential benefits.
Mesh Exposure Leading to Chronic Pain and Dysfunction
Mesh exposure, one of the most common complications following transvaginal mesh placement, occurs when the synthetic mesh erodes through tissue boundaries and becomes exposed in places where it shouldn’t be.
This erosion process often begins gradually as the mesh arms tighten or contract, pulling against sensitive internal structures and creating increasing tension.
The cause of pain associated with transvaginal mesh is frequently related to contracture of the mesh body where the mesh arms are fixed and come under increased tension as the mesh body contracts, creating a painful situation for patients.

Complications reported by women experiencing mesh erosion typically include, but are not limited to:
- Constant or activity-triggered pelvic and vagina pain that worsens over time
- Recurrent urethral infections that resist antibiotic treatment
- Pain during sexual intercourse, often making intimacy impossible
- Abnormal vaginal discharge and bleeding unrelated to menstruation
- Organs perforation when mesh erodes into bladder, rectum, or urethra
- Other severe health conditions and injuries
When Mesh Removal Surgery Becomes Necessary
For many women suffering from transvaginal mesh complications, surgical procedure becomes the only viable option for relief, yet mesh removal carries its own considerable risks.
The difficulties of removal surgery stem from the way mesh integrates with other tissues and the proximity of the material to important structures like the pubic bone and vital organs.
As medical experts explain, transvaginal mesh removal used to treat pelvic organ prolapse is the most technically difficult due to the larger amount of mesh used and its position close to important organs like the urethra, bladder, and bowel.
Complete mesh removal presents major challenges for surgeons and patients alike, often requiring further surgery and specialized expertise not available in all medical centers.
As noted by specialists, the problem is particularly challenging because transvaginal mesh placed for prolapse is relatively easy to put in, but very difficult to remove mesh due to the way it is anchored to bones and ligaments in the leg and pelvis.
Even after mesh removal surgery, many women continue to experience chronic pain and dysfunction, as nerve damage and tissue scarring may persist indefinitely, creating a lasting legacy of physical impairment that requires comprehensive ongoing care and pain management strategies.
Emotional and Social Effects of Mesh Complications
Beyond the physical symptoms, transvaginal mesh complications can devastate a woman’s emotional wellbeing and social functioning, creating a cascade of psychological impacts that compound the physical suffering.

The chronic nature of mesh-related pain and dysfunction forces many women to dramatically alter their daily activities, relationships, and self-perception, often leading to profound feelings of loss and grief for their former lifestyles and capabilities.
Intimate Relationship Changes Due to Pelvic Floor Damage
Mesh complications can profoundly alter a woman’s ability to engage in physical intimacy, creating strain within romantic relationships and affecting both emotional connection and sexual expression.
The persistent pain, vaginal wall damage, and psychological trauma associated with taking depo provera and other treatments for these complications can make sexual activity unbearably painful or impossible.
Qualitative research has revealed that women experiencing mesh complications frequently report reduced sexual functioning and intimacy as a direct result of their physical symptoms.
Weight gain and changes in body image following mesh complications and surgical removal further compound intimacy issues, as women may feel less attractive or desirable.
Most patients struggle to understand the extent of the physical limitations imposed on them, including restrictions on heavy lifting and various physical activities.
Some relationships eventually break down under this pressure, while others adapt through alternative forms of intimacy and closeness, requiring extensive emotional work and communication from both partners to maintain connection despite the physical barriers imposed by mesh complications.
Depression and Anxiety from Chronic Mesh Complications
The persistent and unpredictable nature of transvaginal mesh complications can trigger severe psychological distress, often manifesting as clinical depression and anxiety disorders that further diminish quality of life.
Living with unrelenting pain, dealing with medical systems, and managing disruptions to work, family responsibilities, and social activities can overwhelm even the most resilient individuals.
Research has documented that women with complications from the midurethral sling frequently experience psychologically traumatic effects, including feelings of increased anxiety and fears relating to suicidal thoughts.

Psychological symptoms reported by women with mesh complications often include:
- Persistent feelings of sadness, hopelessness, and worthlessness
- Excessive worry about future health outcomes and treatment options
- Panic attacks, especially before medical appointments or procedures
- Social withdrawal and isolation from friends and family
- Anger and resentment toward healthcare providers who performed the initial surgery
- Post-traumatic stress symptoms related to medical procedures and pain
- Identity loss and grieving for former capabilities and lifestyle
Many women report feeling betrayed by the medical system that was supposed to help them, especially when their symptoms are dismissed or minimized by healthcare providers unfamiliar with complications from this type of mesh used to treat pelvic organ prolapse.
This sense of abandonment can intensify feelings of helplessness and despair, creating a cycle where psychological distress heightens physical pain perception, which in turn worsens emotional symptoms.
Support groups provide valuable assistance for patients concerned about the recurrence of symptoms after revision surgeries, as well as pain that can radiate to the groin, stomach, and lower back.
Through these connections, many women find that communicating with others who understand the complications of a failed mesh sling helps them discover renewed purpose in raising awareness and advocating for improved mesh complication recognition and treatment, finding meaning amidst their suffering by helping others facing similar challenges.
TruLaw: Accepting Clients for the Transvaginal Mesh Lawsuit
Transvaginal mesh lawsuits are being filed by women across the country who suffered serious complications from pelvic mesh implants used to treat pelvic organ prolapse and stress urinary incontinence.
TruLaw is currently accepting clients for the Transvaginal Mesh lawsuit.
A few reasons to choose TruLaw for your Transvaginal Mesh lawsuit include:
- If We Don’t Win, You Don’t Pay: The Transvaginal Mesh lawyers at TruLaw and our partner firms operate on a contingency fee basis, meaning we only get paid if you win.
- Expertise: We have decades of experience handling product liability cases similar to the Transvaginal Mesh lawsuit.
- Successful Track Record: TruLaw and our partner law firms have helped our clients recover billions of dollars in compensation through verdicts and negotiated settlements.
If you or a loved one suffered pain, infection, bleeding, organ damage, or other complications after receiving a transvaginal mesh implant, you may be eligible to seek compensation.
Contact TruLaw using the chat on this page to receive an instant case evaluation that can determine if you qualify for the Transvaginal Mesh lawsuit today.
Transvaginal Mesh Lawsuit Frequently Asked Questions
-
Women experiencing painful physical symptoms, requiring revision surgeries, or suffering long-term health issues following transvaginal mesh implantation may qualify for legal compensation through a transvaginal mesh lawsuit.
If you or a loved one suffered pain, infection, bleeding, organ damage, or other complications after receiving a transvaginal mesh implant, you may be eligible to seek compensation.
Contact TruLaw using the chat on this page to receive an instant case evaluation that can determine if you qualify for the Transvaginal Mesh lawsuit today.
-
Transvaginal mesh complications may include bleeding, infection, pain during intercourse, difficulty emptying the bladder, urinary tract infections, and recurrent stress incontinence.
Many women also experience emotional distress and a return of pelvic organ prolapse that the mesh was intended to correct.
-
Mesh erosion symptoms include chronic pelvic pain, vaginal bleeding or discharge, and visible or palpable mesh through vaginal tissue.
When erosion occurs in the bowel, patients may experience abdominal pain, vomiting, digestive tract hemorrhage, bowel perforation, or intestinal obstruction that requires immediate medical attention.
-
Pelvic mesh complications include mesh erosion or extrusion through vaginal walls, vaginal scarring, painful fistula formation, dyspareunia (painful intercourse), bladder infections or perforations, and bowel trauma.
Many women also report chronic pelvic, back, and leg pains that significantly impact quality of life.
-
Alternatives to transvaginal mesh include native tissue repair using the patient’s own tissues, biological graft repairs sourced from human or animal tissue, and pubovaginal slings created from the patient’s tissue.
These options may reduce complications while still providing support for pelvic organ prolapse.
-
Yes, transvaginal mesh complications can emerge years after the initial surgery.
Late-onset symptoms may include chronic pain, recurrent infections, mesh contraction causing organ displacement, and erosion into surrounding tissues.
Regular follow-ups are essential even for patients who initially recover without issues.
-
Mesh complications following hysterectomy may include vaginal vault prolapse, mesh erosion into the surgical site, pelvic pain, and infection.
These complications can be particularly challenging to treat because the mesh may be integrated with healing tissues from the hysterectomy, potentially requiring revision surgery.

Managing Attorney & Owner
With over 25 years of legal experience, Jessica Paluch-Hoerman is an Illinois lawyer, a CPA, and a mother of three. She spent the first decade of her career working as an international tax attorney at Deloitte.
In 2009, Jessie co-founded her own law firm with her husband – which has scaled to over 30 employees since its conception.
In 2016, Jessie founded TruLaw, which allows her to collaborate with attorneys and legal experts across the United States on a daily basis. This hypervaluable network of experts is what enables her to share the most reliable, accurate, and up-to-date legal information with our readers!
Additional Transvaginal Mesh Lawsuit resources on our website:
Here, at TruLaw, we’re committed to helping victims get the justice they deserve.
Alongside our partner law firms, we have successfully collected over $3 Billion in verdicts and settlements on behalf of injured individuals.
Would you like our help?
At TruLaw, we fiercely combat corporations that endanger individuals’ well-being. If you’ve suffered injuries and believe these well-funded entities should be held accountable, we’re here for you.
With TruLaw, you gain access to successful and seasoned lawyers who maximize your chances of success. Our lawyers invest in you—they do not receive a dime until your lawsuit reaches a successful resolution!
AFFF Lawsuit claims are being filed against manufacturers of aqueous film-forming foam (AFFF), commonly used in firefighting.
Claims allege that companies such as 3M, DuPont, and Tyco Fire Products failed to adequately warn users about the potential dangers of AFFF exposure — including increased risks of various cancers and diseases.
Depo Provera Lawsuit claims are being filed by individuals who allege they developed meningioma (a type of brain tumor) after receiving Depo-Provera birth control injections.
A 2024 study found that women using Depo-Provera for at least 1 year are five times more likely to develop meningioma brain tumors compared to those not using the drug.
Suboxone Tooth Decay Lawsuit claims are being filed against Indivior, the manufacturer of Suboxone, a medication used to treat opioid addiction.
Claims allege that Indivior failed to adequately warn users about the potential dangers of severe tooth decay and dental injuries associated with Suboxone’s sublingual film version.
Social Media Harm Lawsuits are being filed against social media companies for allegedly causing mental health issues in children and teens.
Claims allege that companies like Meta, Google, ByteDance, and Snap designed addictive platforms that led to anxiety, depression, and other mental health issues without adequately warning users or parents.
Transvaginal Mesh Lawsuits are being filed against manufacturers of transvaginal mesh products used to treat pelvic organ prolapse (POP) and stress urinary incontinence (SUI).
Claims allege that companies like Ethicon, C.R. Bard, and Boston Scientific failed to adequately warn about potential dangers — including erosion, pain, and infection.
Bair Hugger Warming Blanket Lawsuits involve claims against 3M — alleging their surgical warming blankets caused severe infections and complications (particularly in hip and knee replacement surgeries).
Plaintiffs claim 3M failed to warn about potential risks — despite knowing about increased risk of deep joint infections since 2011.
Baby Formula NEC Lawsuit claims are being filed against manufacturers of cow’s milk-based baby formula products.
Claims allege that companies like Abbott Laboratories (Similac) and Mead Johnson & Company (Enfamil) failed to warn about the increased risk of necrotizing enterocolitis (NEC) in premature infants.
Here, at TruLaw, we’re committed to helping victims get the justice they deserve.
Alongside our partner law firms, we have successfully collected over $3 Billion in verdicts and settlements on behalf of injured individuals.
Would you like our help?