FAQ: Are Transvaginal Mesh and Vaginal Mesh the Same?
- Last Updated: June 12th, 2025

Attorney Jessica Paluch-Hoerman, founder of TruLaw, has over 28 years of experience as a personal injury and mass tort attorney, and previously worked as an international tax attorney at Deloitte. Jessie collaborates with attorneys nationwide — enabling her to share reliable, up-to-date legal information with our readers.
Legally Reviewed
This article has been written and reviewed for legal accuracy and clarity by the team of writers and legal experts at TruLaw and is as accurate as possible. This content should not be taken as legal advice from an attorney. If you would like to learn more about our owner and experienced injury lawyer, Jessie Paluch, you can do so here.
Fact-Checked
TruLaw does everything possible to make sure the information in this article is up to date and accurate. If you need specific legal advice about your case, contact us by using the chat on the bottom of this page. This article should not be taken as advice from an attorney.
Key takeaways:
- Transvaginal mesh and vaginal mesh are terms used interchangeably to refer to the same medical device.
- Both terms describe a mesh implant used to treat pelvic organ prolapse (POP) and stress urinary incontinence (SUI) in women. It is also frequently used to treat pelvic floor disorders
- The mesh is surgically implanted through the vagina to provide support to weakened or damaged pelvic organs.
- However, the use of transvaginal mesh has been associated with various complications and adverse effects, leading to numerous lawsuits and regulatory actions.
Overview of Transvaginal Mesh and Vaginal Mesh
Question: Are Transvaginal Mesh and Vaginal Mesh the Same?
Answer: While Transvaginal Mesh and Vaginal Mesh are both used to treat conditions like pelvic organ prolapse and stress urinary incontinence, they differ in terms of their application and associated risks.
On this page, we’ll discuss this question in further depth, an overview of Transvaginal Mesh and Vaginal Mesh, the potential risks and complications associated with Surgical Mesh Implants, and much more.
Understanding Transvaginal Mesh and Vaginal Mesh
Despite numerous settlements, thousands of cases remain pending, the ongoing Transvaginal Mesh Lawsuits involve allegations of negligence, failure to warn about potential risks, and other misconduct by the manufacturers.
Transvaginal mesh is inserted through the vagina and has been associated with a higher risk of complications.
Transvaginal mesh and vaginal mesh are medical devices typically used to provide additional support when repairing weakened or damaged tissue.
Transvaginal mesh and vaginal mesh devices may seem similar, but the applications and associated risk profiles vary significantly:
- Transvaginal Mesh: synthetic mesh inserted through the vagina to treat pelvic organ prolapse and stress urinary incontinence. Its sale has been banned for pelvic prolapse repair due to its association with a higher risk of complications compared to other types of vaginal mesh.
- Vaginal Mesh: a broader term referring to any mesh used in the vaginal area, and is not necessarily inserted transvaginal. It encompasses various types of meshes that may be used for different purposes, such as providing support during tissue repair or addressing other gynecological issues.
It’s important to note that the sale of transvaginal mesh devices for pelvic organ prolapse repair has been halted due to safety concerns after the FDA reviewed their premarket approval (PMA) applications, stating that the manufacturers did not provide adequate evidence to demonstrate a reasonable assurance of safety and effectiveness for these devices.
Table of Contents
Understanding Transvaginal Mesh
This synthetic material helps to support weakened or damaged tissue surrounding the pelvic organs; however, various complications can arise from its use.

Several manufacturers produce this mesh with differing brands available on the market.
Transvaginal mesh alternatives exist outside of opting for implants, such as native tissue repair or biologic meshes derived from animal tissues.
What is Transvaginal Mesh?
Transvaginal mesh is a medical device commonly used in surgeries to treat conditions like stress urinary incontinence (SUI) and pelvic organ prolapse (POP).
It involves making an incision in the vaginal wall, through which the mesh is inserted, offering much-needed support for weakened or damaged tissue.
Made of absorbable or permanent material, this surgical mesh provides reinforcement to the vaginal wall and bladder.
Despite its prevalent usage, there have been higher instances of problems related to transvaginal mesh compared to other treatments.
Therefore, it’s imperative for women considering this procedure to fully understand its potential benefits and risks.
Uses of Transvaginal Mesh
When the pelvic floor weakens, it can no longer adequately support pelvic organs like the bladder or uterus.
This lack of support causes these organs to drop, a condition known as POP.
Transvaginal mesh provides much-needed reinforcement to the weakened vaginal walls.
Another common use of this product is for SUI treatment.
This condition leads to unintentional urine leakage when pressure increases on the bladder due to actions like laughing, sneezing or exercising.
Surgeons implant transvaginal mesh as a sling around the urethra or bladder neck, thereby controlling involuntary urine flow.
Unlike traditional surgery methods that use stitches alone, surgeons turn to synthetic polypropylene meshes because they offer increased durability and strength after being surgically implanted through the vagina.
Complications with Transvaginal Mesh Implants
Unfortunately, these implants come with a range of complications that can cause significant discomfort and potential health risks.
The most common problem faced by patients is pain, which could be due to the implant itself or as a result of surgical procedures.
One serious concern associated with transvaginal mesh implants is mesh erosion—an issue flagged by the FDA due to its frequency among patients.
Mesh erosion occurs when the synthetic materials used in these devices wear away at surrounding tissues.
Symptoms of Mesh Erosion commonly include, but are not limited to:
- Severe inflammation
- Tissue damage
- Infections
- Sepsis
This condition often requires additional surgery for correction or removal of the eroded material.
Additionally, during the placement procedure for transvaginal mesh devices, there’s an inherent risk of injury to adjacent organs like the bladder or bowel which might require immediate medical intervention.
Ultimately, monitoring these potential difficulties plays a crucial role in ensuring patient safety post-implantation process while managing pelvic floor disorders effectively.
Manufacturers and Brands of Transvaginal Mesh
Several companies manufacture transvaginal meshes, including global medical device providers.
These manufacturers design and produce a variety of mesh brands to suit different patient needs and complications.
One such brand is Boston Scientific’s Advantage Sling System, utilized widely for its effectiveness in treating pelvic organ prolapse and stress urinary incontinence.
However, after the FDA directive in 2019 barring the sale of these devices for transvaginal repair of pelvic organ prolapse within the United States, many products are no longer available domestically.
Despite these changes in availability, numerous other brands of this vital device exist worldwide with similar designs and functionalities.
Alternatives to Transvaginal Mesh
Exploring alternatives to transvaginal mesh is crucial for women seeking treatment for conditions like pelvic organ prolapse and stress urinary incontinence.
Here are some other alternatives to transvaginal mesh that medical professionals may suggest:
- Native Tissue Repair: This surgical procedure uses a woman’s own tissues to support pelvic organs experiencing prolapse.
- Prolapse Repairs without Mesh: Surgeons make repairs using stitches alone, without the addition of synthetic materials or biologic mesh.
- Pessaries: These are non-surgical devices inserted into the vagina to support prolapsed organs.
- Pelvic Floor Therapy: Specialist therapists provide exercises designed to strengthen the pelvic floor muscles.
- Lifestyle modifications: Doctors may recommend changes such as weight loss, bowel management strategies, and quitting smoking.
- Non-Surgical Management with Vaginal Estrogen: This treatment option involves taking estrogen to improve the health of vaginal tissues and potentially slow prolapse progression.
- Laparoscopic Sacrocolpopexy: A minimally invasive surgical technique used for repairing pelvic organ prolapse, usually done with a synthetic polypropylene mesh attached from the cervix or top of the vagina up towards the sacrum (a bone at the base of your spine).
- Mid-Urethral Sling Procedure: It’s primarily used for treating stress urinary incontinence by placing a mesh sling under the urethra to support it and help keep it closed during physical activity.
- Colpocleisis: A procedure done for older adults who aren’t sexually active anymore; it involves closing off or removing parts of their vagina.
Lawsuits Involving Transvaginal Mesh
Transvaginal mesh lawsuits have risen significantly over the years due to numerous complications experienced by patients.
These complications often include severe discomfort, bleeding, infection, and even organ perforation.
The legal claims against companies manufacturing transvaginal mesh accuse them of negligence along with breaches in warranty, and defects in design and manufacturing processes.
One notable settlement among these lawsuits stands as one of the largest to date.
The initiation of most transvaginal mesh lawsuits arose following a 2011 communication from the Food and Drug Administration concerning the use of surgical mesh for pelvic organ prolapse repair.
Consequently, these settlements contributed to an approximate $8 billion payout in personal injury cases related to transvaginal mesh complications.
Potential Complications with Surgical Mesh Implants
Over the years, surgical mesh implants have become associated with a series of potential complications leading to women experiencing a wide range of injuries and health issues.
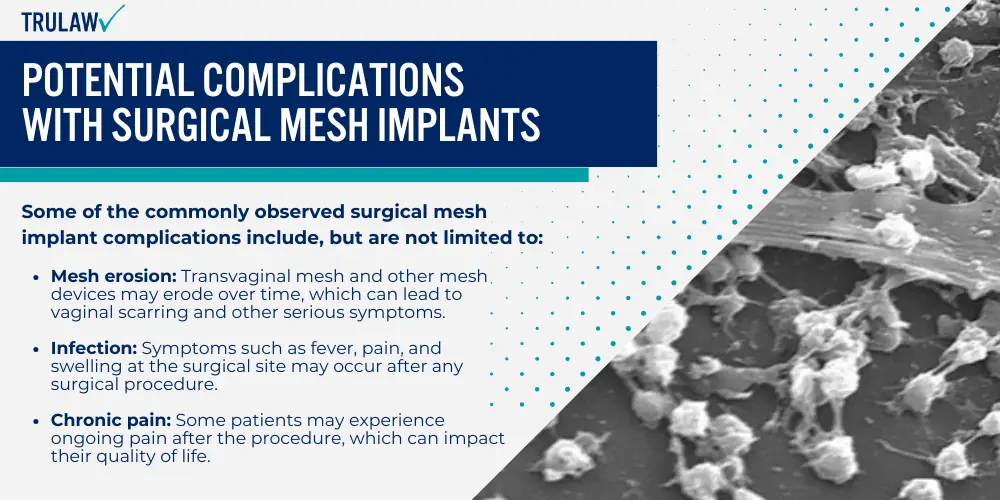
In some cases, these complications may require additional surgery to address.
Complications with Surgical Mesh Implants
Symptoms can occur shortly after the surgery or arise years later, adding to the uncertainty of this medical procedure.
Some of the commonly observed surgical mesh implant complications include, but are not limited to:
- Mesh erosion: Transvaginal mesh and other mesh devices may erode over time, which can lead to vaginal scarring and other serious symptoms.
- Infection: Symptoms such as fever, pain, and swelling at the surgical site may occur after any surgical procedure.
- Chronic pain: Some patients may experience ongoing pain after the procedure, which can impact their quality of life.
Patients might also experience recurring infections due to mesh erosion into surrounding tissue, contributing further to ongoing discomfort and health concerns.
Mesh Erosion
Mesh erosion is a frequent and distressing complication with transvaginal mesh implants.
This occurs when the surgical mesh breaks down and gradually moves through the vaginal wall or into surrounding organs, causing immense discomfort and health complications.
One might experience symptoms such as pain during sexual intercourse, pelvic discomfort, persistent infections, or even bleeding.
Notably, erosion does not happen overnight but may present itself years after the procedure.
The severity of this complication varies from minor irritations to significant injuries requiring additional surgeries for correction.
Moreover, there’s a potential risk of mesh eroding into bowel areas which poses a serious health concern.
Therefore, it’s crucial for women to be aware of such risks before opting for transvaginal mesh surgery and consider alternative treatments if deemed necessary by their healthcare providers.
Infection
Infection is a potential complication associated with transvaginal mesh implants.
The implanted mesh, often made of polypropylene or other synthetic materials, can become a breeding ground for bacteria, leading to an infection.
This happens in approximately 0-8% of all cases and occurs when bacteria colonize the surgical mesh after implantation.
Symptoms may include persistent vaginal bleeding, pain during intercourse or bowel movements, and foul-smelling discharge.
If left untreated, this could lead to serious complications such as pelvic organ prolapse and stress urinary incontinence.
Other Treatment Options for Pelvic Organ Prolapse
Other than Transvaginal Mesh, various non-surgical treatments, and surgical interventions without the use of mesh are potential options for managing pelvic organ prolapse.
Non-surgical Treatments
Non-surgical treatments offer options for addressing pelvic organ prolapse without the need for invasive procedures.
Here are some of these non-surgical approaches to managing pelvic organ prolapse:
- Pelvic Floor Exercises: These exercises strengthen the muscles of your pelvic floor to better support your pelvic organs.
- Estrogen Therapy: Vaginal use of estrogen can help restore strength and elasticity to vaginal tissues.
- Pessary Devices: A doctor can fit these removable devices inside the vagina, providing support to sagging pelvic organs.
- Lifestyle Changes: Losing weight or quitting smoking can reduce pressure on the pelvic muscles, possibly relieving symptoms.
- Bladder Training: This technique helps control urinary incontinence by delaying urination after you get the urge to go.
- Bowel Management: Regular bowel movements reduce strain on the pelvic muscles, which can be attained by a high-fiber diet and drinking plenty of fluids.
- Medications: Certain medicines may be useful in managing symptoms of urinary incontinence.
Surgical Treatments (Without Mesh)
Pelvic organ prolapse and stress urinary incontinence are health conditions that can seriously impact the quality of life for many women.
Surgical treatments without the use of mesh exist which could provide relief to these patients.
- Native tissue repair: involves utilizing a woman’s own ligaments and tissues to restore the pelvic organs to their original position.
- Sacral colpopexy: works particularly well for severe cases of pelvic organ prolapse, where it employs sutures (instead of mesh) to attach the vagina to strong ligaments along the spine.
- Bulking agent injections: used to treat mild stress urinary incontinence by injecting materials around the urethra, helping it stay closed and prevent urine leakage.
- Pessaries Devices: a silicone device inserted into the vagina, providing support while also achieving symptom relief from both pelvic organ prolapse and urinary incontinence.
What to Do If You Have Concerns
If you have concerns about transvaginal mesh, it is imperative to report any complications related to medical devices directly to the FDA.

Seeking Medical Advice
If you’ve experienced vaginal mesh complications, injuries, or adverse effects from a transvaginal mesh implant- you may be eligible to file for the Transvaginal Mesh Lawsuit.
Contact the experienced Transvaginal Mesh Lawyers at TruLaw today for a no-obligation consultation.
We can provide insights on filing a transvaginal mesh lawsuit to help you seek the compensation you deserve.
Consulting an experienced legal professional is critical if you are experiencing symptoms following your procedure.
Reporting to the FDA
If you experience complications from transvaginal mesh, it’s essential to report the situation to the FDA.
Users can submit reports directly through the MedWatch Voluntary Reporting Form available on their website.
This allows the FDA to take timely action against potentially harmful medical devices and protect public safety.
Your experiences and feedback play a crucial role in this process, helping to inform decisions made about these products’ safety and effectiveness.
Always provide as much detail as possible when filing your report, including any symptoms or side effects experienced post-surgery.
Medical professionals are also encouraged to report any observed adverse events related to transvaginal mesh usage.
Is Transvaginal Mesh Banned in Other Countries?
Similar to the United States’ decision, several countries have also taken action against using these implants for similar cases, including Australia, New Zealand, the United Kingdom, France, and Canada.

Before this groundbreaking ban, manufacturers were required to submit premarket approval (PMA) applications providing evidence that their products were safe and effective.
The FDA found that none could adequately demonstrate an acceptable balance between potential benefits and risks associated with these mesh devices.
Countries around the world have different stances on transvaginal mesh use.
The following countries are now following suit in putting stringent measures against using these implants for similar cases:
- Australia
- New Zealand
- United Kingdom
- France
- Canada
Australia and New Zealand stood at the forefront, banning transvaginal mesh products due to concerns over safety and efficacy.
The Australian Therapeutic Goods Association moved against its usage for pelvic organ prolapse (POP) repairs in 2017 following consistent reports of serious complications.
Moreover, the United Kingdom took a similar course as Australia, halting procedures involving vaginal mesh implants for POP in July 2018.
France became another country that decided against using this controversial product by suspending all sales of urogynecological meshes intended for certain surgical treatments of urinary incontinence and POP because of safety issues sparked by numerous lawsuits worldwide.
Canada joined these countries when Health Canada removed transvaginal mesh from its market due to an increasing amount of reported adverse events.
In addition to those mentioned previously, many other countries have taken steps towards restricting or outright prohibiting the use of transvaginal mesh owing to mounting evidence related to risks associated with these devices.
Options to Remove Transvaginal Mesh
Problems with transvaginal mesh may mandate its removal, which can offer relief from complications.

This process, while complex, is typically managed by experienced urogynecologists.
Here are a few options to remove a Transvaginal Mesh device:
- Partial Mesh Removal: This procedure extracts only part of the mesh in cases where only a certain section causes issues. This method might alleviate symptoms without requiring a full extraction.
- Complete Mesh Removal: A comprehensive extraction is needed when complications are severe or widespread across multiple sections of the mesh. A complete removal aims to eradicate all related symptoms.
- Laparoscopic Surgery: In some instances, laparoscopic intervention may be an option. By making small incisions and using specialized tools, doctors can remove the mesh with less physical trauma compared to traditional surgery.
- Vaginal Approach: Surgeons may choose to extract the mesh vaginally if feasible and advantageous for patient recovery.
- Abdominal Approach: If vaginal access proves difficult or inadequate for effective removal, doctors might execute an abdominal surgical approach.
- Combination Therapy: In some cases, hormone treatments like vaginal estrogen might accompany surgical procedures to boost tissue healing post-removal.
Conclusion
Through this article, we have navigated the intricacies of transvaginal and vaginal mesh, examining their unique properties and applications to better understand their differences.
If you’ve experienced vaginal mesh complications, injuries, or adverse effects from a transvaginal mesh implant- you may be eligible to file for the Transvaginal Mesh Lawsuit.
Contact the experienced Transvaginal Mesh Lawyers at TruLaw today for a no-obligation consultation.
We’re here to help you seek the compensation you deserve.
Transvaginal Mesh Lawsuit Frequently Asked Questions
-
Question: Are Transvaginal Mesh and Vaginal Mesh the Same?
Answer: No, Transvaginal Mesh and Vaginal Mesh are not the same, although they are used for similar purposes. Both are synthetic net-like substances used to provide extra support to repair weakened or damaged internal tissue. However, their applications differ.
Key differences between transvaginal mesh and vaginal mesh include:
Transvaginal Mesh:
- Primarily used to treat pelvic organ prolapse and stress urinary incontinence.
- The FDA banned its use for pelvic organ prolapse repair in 2019 due to complications.
- It can still be used for stress urinary incontinence in a sling procedure or in abdominal surgeries to support the vaginal wall.
- There have been no recalls on transvaginal mesh devices, as the FDA ban applies only to pelvic organ prolapse repair.
Vaginal Mesh:
- Primarily used to repair vaginal wall prolapse.
- No reported FDA bans or recalls.
- May be used to treat other gynecological issues, such as vaginal wall prolapse.
-
The implantation of transvaginal mesh involves a surgical procedure performed through the vagina.
The surgeon makes small incisions in the vaginal wall and inserts the mesh to provide support to the weakened pelvic organs.
The mesh is then secured in place using sutures, staples, or other fixation methods.
The procedure aims to restore the normal position and function of the pelvic organs.
-
Transvaginal mesh is primarily used in the treatment of pelvic organ prolapse (POP) and stress urinary incontinence (SUI) in women.
POP occurs when the pelvic organs, such as the bladder, uterus, or rectum, descend or protrude into the vaginal wall.
SUI, on the other hand, is the involuntary leakage of urine during activities that increase abdominal pressure, such as coughing, sneezing, or exercising.
Transvaginal mesh provides support to the weakened tissues and helps alleviate the symptoms of these conditions.
-
The use of transvaginal mesh has been associated with various complications and adverse effects.
These can include:
- Mesh erosion: The mesh may erode through the vaginal wall, causing pain, discomfort, and infection.
- Infection: The implantation of mesh carries a risk of infection, which can lead to further complications.
- Pain: Some women may experience chronic pelvic pain or pain during sexual intercourse after the implantation of transvaginal mesh.
- Mesh contraction: The mesh may shrink or contract over time, leading to discomfort and a recurrence of symptoms.
- Organ perforation: In rare cases, the mesh may perforate nearby organs, such as the bladder or rectum.
- Revision surgery: Due to complications or mesh failure, some women may require additional surgeries to remove or repair the mesh.
-
Vaginal mesh and transvaginal mesh are essentially the same medical device, but the terms are used interchangeably.
The difference lies in the way the terms are used.
‘Vaginal mesh’ is a broader term that encompasses all types of mesh implants used in the treatment of POP and SUI, including those implanted through other surgical approaches.
‘Transvaginal mesh’ specifically refers to mesh implants that are inserted through the vagina.
-
Transvaginal mesh removal is a surgical procedure to remove a mesh implant that was previously placed to treat pelvic organ prolapse or stress urinary incontinence.
The procedure is performed to address complications or side effects associated with the mesh, such as pain, infection, erosion, or organ perforation.

Managing Attorney & Owner
With over 25 years of legal experience, Jessica Paluch-Hoerman is an Illinois lawyer, a CPA, and a mother of three. She spent the first decade of her career working as an international tax attorney at Deloitte.
In 2009, Jessie co-founded her own law firm with her husband – which has scaled to over 30 employees since its conception.
In 2016, Jessie founded TruLaw, which allows her to collaborate with attorneys and legal experts across the United States on a daily basis. This hypervaluable network of experts is what enables her to share the most reliable, accurate, and up-to-date legal information with our readers!
Additional Transvaginal Mesh Lawsuit resources on our website:
Here, at TruLaw, we’re committed to helping victims get the justice they deserve.
Alongside our partner law firms, we have successfully collected over $3 Billion in verdicts and settlements on behalf of injured individuals.
Would you like our help?
At TruLaw, we fiercely combat corporations that endanger individuals’ well-being. If you’ve suffered injuries and believe these well-funded entities should be held accountable, we’re here for you.
With TruLaw, you gain access to successful and seasoned lawyers who maximize your chances of success. Our lawyers invest in you—they do not receive a dime until your lawsuit reaches a successful resolution!
AFFF Lawsuit claims are being filed against manufacturers of aqueous film-forming foam (AFFF), commonly used in firefighting.
Claims allege that companies such as 3M, DuPont, and Tyco Fire Products failed to adequately warn users about the potential dangers of AFFF exposure — including increased risks of various cancers and diseases.
Depo Provera Lawsuit claims are being filed by individuals who allege they developed meningioma (a type of brain tumor) after receiving Depo-Provera birth control injections.
A 2024 study found that women using Depo-Provera for at least 1 year are five times more likely to develop meningioma brain tumors compared to those not using the drug.
Suboxone Tooth Decay Lawsuit claims are being filed against Indivior, the manufacturer of Suboxone, a medication used to treat opioid addiction.
Claims allege that Indivior failed to adequately warn users about the potential dangers of severe tooth decay and dental injuries associated with Suboxone’s sublingual film version.
Social Media Harm Lawsuits are being filed against social media companies for allegedly causing mental health issues in children and teens.
Claims allege that companies like Meta, Google, ByteDance, and Snap designed addictive platforms that led to anxiety, depression, and other mental health issues without adequately warning users or parents.
Transvaginal Mesh Lawsuits are being filed against manufacturers of transvaginal mesh products used to treat pelvic organ prolapse (POP) and stress urinary incontinence (SUI).
Claims allege that companies like Ethicon, C.R. Bard, and Boston Scientific failed to adequately warn about potential dangers — including erosion, pain, and infection.
Bair Hugger Warming Blanket Lawsuits involve claims against 3M — alleging their surgical warming blankets caused severe infections and complications (particularly in hip and knee replacement surgeries).
Plaintiffs claim 3M failed to warn about potential risks — despite knowing about increased risk of deep joint infections since 2011.
Baby Formula NEC Lawsuit claims are being filed against manufacturers of cow’s milk-based baby formula products.
Claims allege that companies like Abbott Laboratories (Similac) and Mead Johnson & Company (Enfamil) failed to warn about the increased risk of necrotizing enterocolitis (NEC) in premature infants.
Here, at TruLaw, we’re committed to helping victims get the justice they deserve.
Alongside our partner law firms, we have successfully collected over $3 Billion in verdicts and settlements on behalf of injured individuals.
Would you like our help?