FAQ: What is Transvaginal Mesh Used For?
- Last Updated: July 14th, 2025

Attorney Jessica Paluch-Hoerman, founder of TruLaw, has over 28 years of experience as a personal injury and mass tort attorney, and previously worked as an international tax attorney at Deloitte. Jessie collaborates with attorneys nationwide — enabling her to share reliable, up-to-date legal information with our readers.
Legally Reviewed
This article has been written and reviewed for legal accuracy and clarity by the team of writers and legal experts at TruLaw and is as accurate as possible. This content should not be taken as legal advice from an attorney. If you would like to learn more about our owner and experienced injury lawyer, Jessie Paluch, you can do so here.
Fact-Checked
TruLaw does everything possible to make sure the information in this article is up to date and accurate. If you need specific legal advice about your case, contact us by using the chat on the bottom of this page. This article should not be taken as advice from an attorney.
Key takeaways:
- Transvaginal mesh is a medical tool that helps with pelvic floor disorders and stress urinary incontinence.
- The mesh comes in many forms, made from different materials like polypropylene or animal tissue.
- It's used when non - surgical treatments don't work well enough.
- There can be complications with transvaginal mesh, such as chronic pelvic pain or problems with the mesh eroding into tissues.
What is Transvaginal Mesh Used for? Let's Discuss.
Question: What is Transvaginal Mesh Used for?
Answer: Transvaginal mesh is a surgical device that provides additional support when repairing weakened or damaged tissue. It has been used primarily for two urogynecologic procedures:
The use of Transvaginal Mesh for pelvic organ prolapse repair procedures has been associated with a high risk of complications, leading to the FDA’s decision to halt its sale for this specific procedure.
Transvaginal Mesh-specific Complications & Injuries
Erosion of mesh slings through the vagina is the most commonly reported mesh-specific complication from SUI surgeries with mesh.

The complications associated with transvaginal mesh can include bleeding, infection, mesh erosion, nerve damage, and organ perforation.
The average reported rate of mesh erosion at one year following SUI surgery with mesh is approximately 2 percent.
If you’ve experienced vaginal mesh complications, injuries, or adverse effects from a transvaginal mesh implant- you may be eligible to file for the Transvaginal Mesh Lawsuit.
Contact the experienced Transvaginal Mesh Lawyers at TruLaw today for a no-obligation consultation.
We’re here to help you seek the compensation you deserve.
Table of Contents
What is Transvaginal Mesh Used for?
Transvaginal mesh is a piece of surgical netting that’s used to reinforce the vaginal wall and support pelvic organs in women dealing with pelvic floor disorders, most notably pelvic organ prolapse and stress urinary incontinence.
This synthetic or biologic mesh is designed from materials such as polypropylene or animal tissue, offering diverse options for patients based on their unique needs.
Definition and Purpose
The purpose of this mesh is to provide support and reinforcement for weakened or damaged tissue.
By bolstering the pelvic organs and vaginal wall, it helps reduce discomfort, improve functionality, and enhance quality of life for affected women.
Despite potential complications, experts deem careful positioning of the transvaginal mesh safe, while stating that its use often results in lower rates of repeat surgeries for prolapse compared to other treatments.
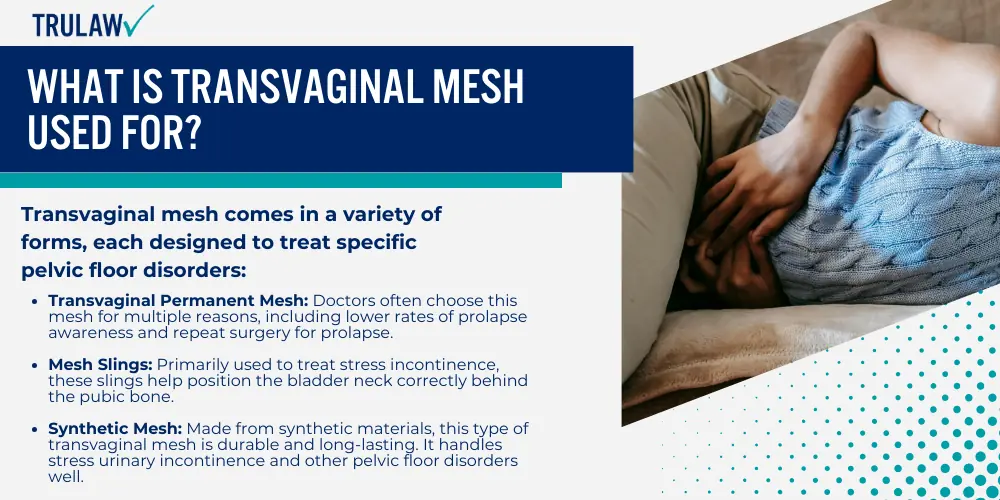
Types of Transvaginal Mesh
Transvaginal mesh comes in a variety of forms, each designed to treat specific pelvic floor disorders:
- Transvaginal Permanent Mesh: Doctors often choose this mesh for multiple reasons, including lower rates of prolapse awareness and repeat surgery for prolapse.
- Mesh Slings: Primarily used to treat stress incontinence, these slings help position the bladder neck correctly behind the pubic bone.
- Synthetic Mesh: Made from synthetic materials, this type of transvaginal mesh is durable and long-lasting. It handles stress urinary incontinence and other pelvic floor disorders well.
- Biologic Mesh: Biological mesh devices have received FDA approval based on their “substantial equivalence” to synthetic meshes, bypassing the standard clinical trial process. Studies on these devices have inconsistently reported clinical outcomes like infection rates.
- Type I Monofilament Mesh: This large-pore polypropylene mesh primarily aids in treating pelvic organ prolapse. It effectively offers support to weakened vaginal walls.
How is Transvaginal Mesh Used?
Transvaginal mesh is commonly used for treating pelvic organ prolapse and stress urinary incontinence.
While effective in many cases, it’s crucial to weigh the benefits against potential risks and consider alternative treatments.
Treating Stress Urinary Incontinence
Transvaginal mesh is instrumental in treating stress urinary incontinence, a condition characterized by uncontrolled urine leakage during physical activities.
Surgical techniques like the mid-urethral sling procedure have proven effective, especially when stress urinary incontinence coexists with pelvic organ prolapse.
In such cases, an anterior vaginal repair surgery, or colporrhaphy, may also be performed.
Considerations Before Surgery
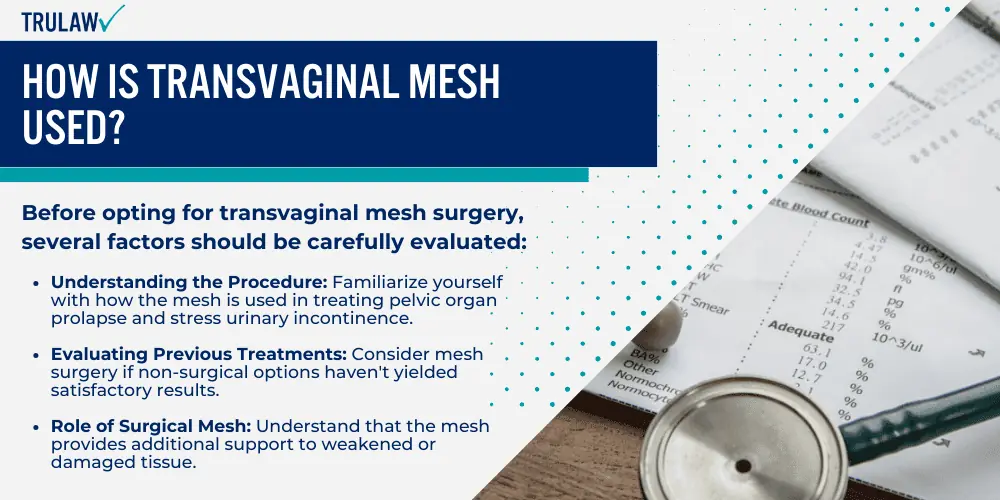
Before opting for transvaginal mesh surgery, several factors should be carefully evaluated:
- Understanding the Procedure: Familiarize yourself with how the mesh is used in treating pelvic organ prolapse and stress urinary incontinence.
- Evaluating Previous Treatments: Consider mesh surgery if non-surgical options haven’t yielded satisfactory results.
- Role of Surgical Mesh: Understand that the mesh provides additional support to weakened or damaged tissue.
- Compared with Native Tissue Repair: Transvaginal mesh has lower rates of repeat surgery and prolapse on examination compared to native tissue repairs.
- Types of Surgery: Abdominal POP surgery using mesh generally has lower complication rates than transvaginal POP surgery.
- Potential Risks: The FDA warns of higher risks associated with transvaginal POP mesh repair compared to native tissue procedures.
- Post-Surgery Symptoms: Be aware of potential post-operative symptoms like pelvic or groin pain and bowel movement issues.
- Reoperation Possibilities: Understand that mesh removal may be necessary in the event of severe complications.
- Post-Operative Care: Regular check-ups are essential for monitoring recovery.
- Legal Considerations: Be informed about potential legal issues and lawsuits related to surgical mesh implants.
Alternatives to Transvaginal Mesh
For those seeking alternatives, several options are available:
- Non-surgical treatments: Such as pelvic floor physical therapy or pessaries.
- Native Tissue Repair: Utilizes the patient’s own tissues instead of synthetic materials.
- Laparoscopic Sacrocolpopexy: A minimally invasive technique for prolapse repairs without using mesh.
- Bladder Neck Suspension: Redirects the urethra and bladder neck towards the pubic bone.
- Urethral Sling Procedures: A small incision allows for the installation of a sling around the bladder neck, reinforcing weakened vaginal wall structures.
Transvaginal mesh surgery can be an effective treatment for pelvic organ prolapse and stress urinary incontinence.
However, it’s crucial to consider the associated risks, FDA warnings, and potential need for reoperations.
Transvaginal mesh alternative treatments are available and should be considered based on individual health status and treatment history.
When is Transvaginal Mesh Used?
Transvaginal mesh is often considered when non-surgical treatments for pelvic organ prolapse and stress urinary incontinence prove ineffective.
While this surgical option aims to reinforce weakened vaginal walls and restore normal function, it’s crucial to assess the potential benefits and risks.
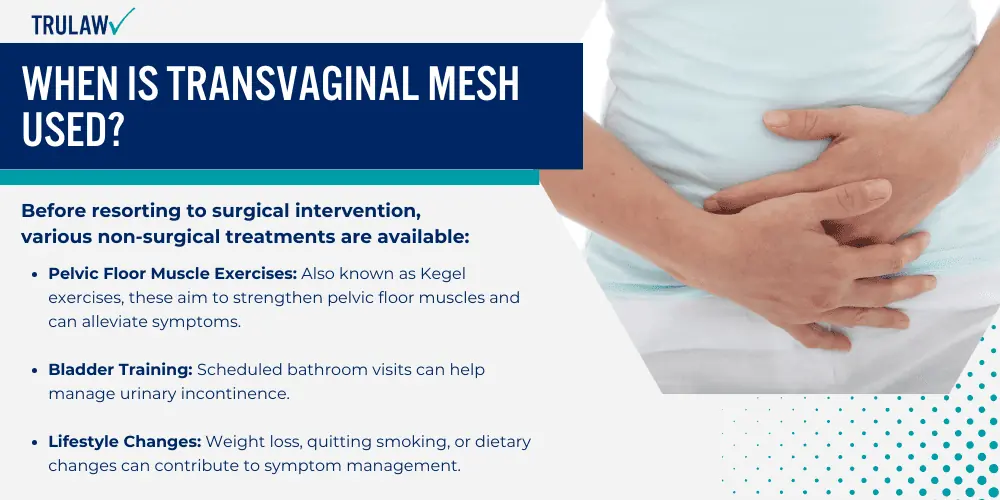
Non-Surgical Treatment Options
Before resorting to surgical intervention, various non-surgical treatments are available:
- Pelvic Floor Muscle Exercises: Also known as Kegel exercises, these aim to strengthen pelvic floor muscles and can alleviate symptoms.
- Bladder Training: Scheduled bathroom visits can help manage urinary incontinence.
- Lifestyle Changes: Weight loss, quitting smoking, or dietary changes can contribute to symptom management.
- Medication: Certain drugs can improve bladder control.
- Pessaries: These devices support prolapsed organs and can relieve pain.
- Biofeedback: Real-time monitoring helps improve muscle control.
- Collagen Injections: Primarily used for stress incontinence, this procedure thickens the urethral or bladder wall.
Limitations of Non-Surgical Treatments
Non-surgical treatments can sometimes fall short, particularly in the following scenarios:
- Pelvic Floor Exercises: May be insufficient if pelvic muscles are significantly weakened.
- Pessary Devices: Require regular cleaning and can cause discomfort.
- Lifestyle Changes: May not yield the desired results despite diligent efforts.
- Bladder Training: Not always effective, especially in severe cases.
- Medication: This may have side effects or lack efficacy.
Surgical Intervention: Transvaginal Mesh
Transvaginal mesh surgery is typically considered when non-surgical options fail to provide adequate relief.
The procedure aims to reinforce weakened vaginal walls and restore normal function.
However, it’s essential to weigh the potential benefits against the risks, including possible complications and the need for reoperations.
Complications of Transvaginal Mesh Implants
Transvaginal mesh has been a subject of increasing scrutiny, particularly due to rising safety concerns and subsequent FDA bans.
While the mesh is designed to treat pelvic organ prolapse and urinary issues, the complications arising from its use have led many surgeons to reconsider its application.
Safety Concerns and FDA Ban
The FDA has imposed a ban on the use of transvaginal mesh for pelvic organ prolapse due to a surge in reported complications.
Issues such as vaginal scarring, debilitating pain, and other severe complications have led to increased scrutiny and the eventual withdrawal of these products from the market.
These complications have been observed across all brands of surgical mesh used for pelvic organ repairs.
Symptoms of Mesh Complications
It’s crucial for patients to be aware of the symptoms that may indicate complications from transvaginal mesh implants:
- Unusual Vaginal Bleeding or Discharge: Often an early sign of complications.
- Pelvic Discomfort and Swelling: May range from mild to severe pain, often accompanied by inflammation.
- Pain During Intercourse: Indicates potential mesh erosion affecting both partners.
- Bladder and Bowel Issues: May disrupt regular bladder and bowel functions.
- Frequent Infections: Due to foreign body reactions to the implanted material.
- Return of Prolapse or Incontinence: This could signify failed treatment or mesh erosion.
- Tearing of Tissues and Organs: In severe cases, this leads to significant internal damage.
Potential Reoperations
Complications from transvaginal mesh implants may necessitate additional surgical interventions. Here are some scenarios that may require reoperation:
- Mesh Erosion: This leads to pain and discomfort, often requiring surgical correction.
- Organ Perforation: Demands immediate medical attention and likely reoperation.
- Recurrence of Prolapse: May necessitate another operation using an alternative treatment option.
- Infections: Severe infections may require removal of the mesh.
- Bleeding and Hematoma: Uncontrolled bleeding or blood clot formation may require further surgical intervention.
- Severe Pain: Persistent or debilitating pain could indicate complications requiring reevaluation and possible reoperation.
- Autoimmune Problems: Though less common, some patients have reported autoimmune issues necessitating additional procedures.
- Mesh Shrinkage: This can lead to vaginal shortening, tightening, or pain, requiring corrective surgery.
- Urinary Tract Disorders: Such as urinary incontinence, may necessitate another operation.
While transvaginal mesh was initially seen as a promising solution for pelvic organ prolapse and urinary issues, the rising number of complications has led to increased scrutiny and an FDA ban.
Patients who have undergone these procedures should be vigilant about recognizing symptoms and consult their healthcare providers for appropriate treatment options, including potential reoperations.
Post-Operative Care and Monitoring
Comprehensive post-operative care and monitoring are vital components for a successful recovery following transvaginal mesh surgery.

Monitoring Post-Operative Symptoms
Postoperative vigilance is crucial to identify any signs of complications.
Here are a few commonly reported post-0perative symptoms to monitor:
- Unusual Vaginal Bleeding or Discharge: Could indicate mesh complications.
- Recurrent Urinary Tract Infections: May be related to the surgical procedure.
- Persistent Pelvic or Groin Pain: A sign of potential complications.
- Difficulty During Bowel Movements: This could be related to mesh placement.
- Signs of Mesh Exposure: Such as feeling rough edges in the vagina.
- Pain During Sexual Intercourse: May indicate mesh erosion.
- Incontinence or Difficulty Urinating: This could signify a failed treatment.
Questions to Ask Before Surgery
Before undergoing transvaginal mesh surgery, it’s essential to consult with your healthcare provider.
Consider asking the following questions:
- How Does Transvaginal Mesh Work?: Understand the mechanics of the mesh.
- Purpose of This Mesh Type: Why is this specific mesh recommended for your case?
- Alternatives to Mesh: Are there other treatment options?
- FDA Concerns: How do FDA safety warnings affect your surgery?
- Potential Post-Surgery Complications: Understand the risks and their frequency.
- Plan for Complications: What steps will be taken if complications arise?
- Recovery Time: How long will the recovery process take?
- Post-Surgery Activities: Are there activities to avoid to prevent complications?
- Persistent Symptoms: Could issues like vaginal bleeding or UTIs occur post-surgery?
- Life Changes: How will the surgery affect sexual activity and urinary function?
Importance of Follow-Up Care
Regular appointments with your healthcare provider are crucial for monitoring any potential complications and ensuring a smooth recovery process.
These interactions serve multiple purposes:
- Early Identification: Promptly address issues like persistent vaginal bleeding or discomfort.
- Monitoring: Regular checks help in the early detection of mesh exposure, enhancing patient safety.
- Patient Education: Provides an opportunity for patients to discuss concerns and symptoms with healthcare providers to educate them on optimal recovery steps.
Regular follow-up appointments are indispensable for monitoring recovery and addressing any complications promptly.
Seeking Medical Advice
Early recognition of complications arising from transvaginal mesh implants is crucial for timely intervention.
When to Seek Medical Help
Postoperative symptoms may necessitate urgent medical consultation.
Here are situations that should prompt you to contact your healthcare provider:
- Persistent Pelvic Pain or Discomfort: This could indicate mesh complications.
- Recurrent Urinary Tract Infections: May be related to the surgical procedure.
- Bleeding or Spotting: Beyond the normal healing period.
- Mesh Exposure: Noticeable mesh through the vaginal skin.
- Pain During Sexual Intercourse: May indicate mesh erosion.
- Bowel or Urinary Issues: Problems with bowel movements or passing urine.
- Groin Pain: That persists beyond the expected recovery time.
- Debilitating Pain: An increase in symptom intensity requiring immediate attention.
Further Resources for Information
Empower yourself by exploring multiple sources of information.
Here are some reliable resources:
- Urogynaecological Surgical Mesh Hub: Comprehensive information and support.
- American Urogynecologic Society (AUGS): Patient fact sheets, FAQs, and surgeon directories.
- National Association For Continence (NAFC): Resources on incontinence and pelvic organ prolapse.
- U.S Food and Drug Administration (FDA): Updated safety communications and advisories.
- Mayo Clinic: Medical insights into conditions and risks associated with transvaginal mesh.
- MedlinePlus: Educational materials on female pelvic reconstructive surgery.
Support Services for Mesh Patients
Patients have access to a variety of supportive services:
- Hotline Services: Dedicated hotlines for questions and educational information.
- Counseling and Psychological Support: Emotional and mental health support services.
- Online Forums: Communities for sharing personal experiences and advice.
- Health Education Classes: Comprehensive educational programs on transvaginal mesh.
- Legal Assistance: Crucial for those facing complications and considering legal action.
- Physical Therapy Referrals: Specialized therapists can aid in recovery.
- Patient Advocacy Groups: Organizations advocating for safety practices concerning transvaginal meshes.
Recognizing the signs of complications early and taking advantage of available resources can significantly impact the outcome of transvaginal mesh procedures.
Vaginal Mesh Lawsuits: Ongoing Litigations
The Multidistrict Litigation (MDL) concerning vaginal mesh lawsuits concluded in November 2022.
However, this closure does not preclude individuals from pursuing legal action in state courts.
Individuals who have experienced complications or adverse effects from transvaginal mesh implants may still be eligible to file lawsuits in state courts.
Eligibility for Transvaginal Mesh Lawsuit
If you’ve experienced vaginal mesh complications, injuries, or adverse effects from a transvaginal mesh implant- you may still be eligible to file for the Transvaginal Mesh Lawsuit.
If you fall into this category, it’s crucial to consult with experienced legal professionals to assess your case.
TruLaw offers no-obligation consultations for individuals who believe they may have a valid claim concerning transvaginal mesh complications.
Our team of experienced Transvaginal Mesh Attorneys is equipped to evaluate your case and guide you through the legal process.
Transvaginal Mesh Lawsuit Frequently Asked Questions
-
Question: What is Transvaginal Mesh used for?
Answer: Transvaginal mesh is used in a variety of medical procedures. It is made of synthetic polypropylene and is often used to treat pelvic floor disorders.
However, the use of mesh in transvaginal prolapse repair has been associated with complications, leading to the FDA’s decision to halt its sale for this specific procedure.
Key considerations about Transvaginal Mesh usage include:
- Potential Risks: Transvaginal mesh has been a beneficial treatment for many patients suffering from pelvic floor disorders. However, it is essential to understand that the device comes with its own set of risks. Known complications include bleeding, infection, mesh erosion, nerve damage, and organ perforation.
- FDA Guidelines: In light of the potential risks, the FDA has imposed restrictions on the sale of transvaginal mesh for certain procedures. The most notable restriction is on its use for transvaginal prolapse repair.
-
Surgical mesh is used in the treatment of Pelvic Organ Prolapse (POP) to provide support to the affected organs.
It is inserted in the affected area to restore organ support and relieve pain and pressure in the pelvic area.
The mesh can be implanted through abdominal surgeries to suspend the top of the vagina to a structure on the sacrum.
-
The utilization of pelvic mesh in medical procedures, while beneficial for many, has been associated with a range of complications.
These adverse effects can significantly impact a patient’s quality of life and may necessitate further medical intervention.
Types of Complications
Below is a detailed list of complications that may arise from the use of pelvic mesh:
- Pain: Patients may experience varying degrees of discomfort in the pelvic region post-implantation.
- Erosion: Over time, the mesh may erode the surrounding tissue, leading to further complications.
- Voiding Dysfunction: Difficulty in urinating can be a significant issue for some patients.
- Infection: The implantation of mesh carries an inherent risk of infection.
- Urinary Tract Infections (UTIs): A subset of patients may experience recurring UTIs post-procedure.
- Fistulae: The mesh can lead to the formation of abnormal connections between organs.
- Organ Perforation: In severe cases, the mesh may puncture surrounding organs, requiring immediate medical attention.
- Bleeding: Some patients may experience bleeding as a result of the mesh implant.
- Vaginal Scarring: Scarring in the vaginal area is another potential complication.
- Neuromuscular Alterations: Changes in nerve and muscle function can occur, affecting mobility and sensation.
- Lower Urinary Tract Symptoms: Symptoms such as frequent urination or a sudden, strong urge to urinate may manifest.
- Bowel Complications: The mesh can adversely affect bowel function, leading to digestive issues.
- Immune Disorders: Though less common, the mesh can potentially trigger immune reactions, leading to a range of symptoms.
The use of pelvic mesh is not without risks.
Patients considering this treatment option should be fully informed of the potential complications and consult their healthcare providers for a comprehensive risk assessment.
-
Yes, the FDA has issued several warnings on the use of transvaginal mesh.
These include orders to stop selling and distributing certain mesh products and requirements for manufacturers to conduct postmarket surveillance studies.
The FDA has determined that transvaginal mesh for pelvic organ prolapse (POP) repair presents potential risks and does not have a favorable benefit-risk profile compared to native tissue repair.
As a result, the FDA has reclassified surgical mesh for transvaginal POP repair as a class III device, requiring premarket approval applications.
The FDA continues to provide updates and information to the public about the use of surgical mesh for POP and stress urinary incontinence (SUI).

Managing Attorney & Owner
With over 25 years of legal experience, Jessica Paluch-Hoerman is an Illinois lawyer, a CPA, and a mother of three. She spent the first decade of her career working as an international tax attorney at Deloitte.
In 2009, Jessie co-founded her own law firm with her husband – which has scaled to over 30 employees since its conception.
In 2016, Jessie founded TruLaw, which allows her to collaborate with attorneys and legal experts across the United States on a daily basis. This hypervaluable network of experts is what enables her to share the most reliable, accurate, and up-to-date legal information with our readers!
Additional Transvaginal Mesh Lawsuit resources on our website:
Here, at TruLaw, we’re committed to helping victims get the justice they deserve.
Alongside our partner law firms, we have successfully collected over $3 Billion in verdicts and settlements on behalf of injured individuals.
Would you like our help?
At TruLaw, we fiercely combat corporations that endanger individuals’ well-being. If you’ve suffered injuries and believe these well-funded entities should be held accountable, we’re here for you.
With TruLaw, you gain access to successful and seasoned lawyers who maximize your chances of success. Our lawyers invest in you—they do not receive a dime until your lawsuit reaches a successful resolution!
AFFF Lawsuit claims are being filed against manufacturers of aqueous film-forming foam (AFFF), commonly used in firefighting.
Claims allege that companies such as 3M, DuPont, and Tyco Fire Products failed to adequately warn users about the potential dangers of AFFF exposure — including increased risks of various cancers and diseases.
Depo Provera Lawsuit claims are being filed by individuals who allege they developed meningioma (a type of brain tumor) after receiving Depo-Provera birth control injections.
A 2024 study found that women using Depo-Provera for at least 1 year are five times more likely to develop meningioma brain tumors compared to those not using the drug.
Suboxone Tooth Decay Lawsuit claims are being filed against Indivior, the manufacturer of Suboxone, a medication used to treat opioid addiction.
Claims allege that Indivior failed to adequately warn users about the potential dangers of severe tooth decay and dental injuries associated with Suboxone’s sublingual film version.
Social Media Harm Lawsuits are being filed against social media companies for allegedly causing mental health issues in children and teens.
Claims allege that companies like Meta, Google, ByteDance, and Snap designed addictive platforms that led to anxiety, depression, and other mental health issues without adequately warning users or parents.
Transvaginal Mesh Lawsuits are being filed against manufacturers of transvaginal mesh products used to treat pelvic organ prolapse (POP) and stress urinary incontinence (SUI).
Claims allege that companies like Ethicon, C.R. Bard, and Boston Scientific failed to adequately warn about potential dangers — including erosion, pain, and infection.
Bair Hugger Warming Blanket Lawsuits involve claims against 3M — alleging their surgical warming blankets caused severe infections and complications (particularly in hip and knee replacement surgeries).
Plaintiffs claim 3M failed to warn about potential risks — despite knowing about increased risk of deep joint infections since 2011.
Baby Formula NEC Lawsuit claims are being filed against manufacturers of cow’s milk-based baby formula products.
Claims allege that companies like Abbott Laboratories (Similac) and Mead Johnson & Company (Enfamil) failed to warn about the increased risk of necrotizing enterocolitis (NEC) in premature infants.
Here, at TruLaw, we’re committed to helping victims get the justice they deserve.
Alongside our partner law firms, we have successfully collected over $3 Billion in verdicts and settlements on behalf of injured individuals.
Would you like our help?