FAQ: What Are Common Transvaginal Mesh Complications?
- Last Updated: June 12th, 2025

Attorney Jessica Paluch-Hoerman, founder of TruLaw, has over 28 years of experience as a personal injury and mass tort attorney, and previously worked as an international tax attorney at Deloitte. Jessie collaborates with attorneys nationwide — enabling her to share reliable, up-to-date legal information with our readers.
Legally Reviewed
This article has been written and reviewed for legal accuracy and clarity by the team of writers and legal experts at TruLaw and is as accurate as possible. This content should not be taken as legal advice from an attorney. If you would like to learn more about our owner and experienced injury lawyer, Jessie Paluch, you can do so here.
Fact-Checked
TruLaw does everything possible to make sure the information in this article is up to date and accurate. If you need specific legal advice about your case, contact us by using the chat on the bottom of this page. This article should not be taken as advice from an attorney.
Key takeaways:
- Transvaginal mesh is a surgical device used to support weak tissues in the female pelvic area. It's commonly used for conditions like Pelvic Organ Prolapse and Stress Urinary Incontinence.
- This mesh can be made from synthetic materials or natural animal tissues. Each type comes with its own benefits and potential complications such as mesh erosion and infection.
- Common surgery procedures using transvaginal mesh include Midurethral Sling Procedure, Anterior, and Posterior Vaginal Wall Repair.
- Complications after transvaginal mesh surgery can occur, including painful intercourse, bowel problems, bleeding issues, pelvic pain and recurrence of original condition. Prompt medical attention is recommended if complications arise.
What Are Common Transvaginal Mesh Complications? Lets Discuss.
Question: What are common Transvaginal Mesh complications?
Answer: Transvaginal mesh is a surgical implant used to treat Pelvic Organ Prolapse (POP) and Stress Urinary Incontinence (SUI) in women.
On this page, we’ll provide an overview of the common Transvaginal Mesh complications, recommendations for women considering Transvaginal Mesh surgery, the usage of Transvaginal Mesh, and much more.

Common Transvaginal Mesh Complications
In addition to pain and vaginal mesh erosion, there are other complications that can arise from transvaginal mesh surgery, such as:
- Voiding Dysfunction: Some women may experience difficulty with urination, such as incomplete emptying of the bladder or urinary retention.
- Infection: Infection can occur at the site of the mesh implant, leading to symptoms such as fever, pain, redness, or discharge.
- Bowel Complications: Transvaginal mesh surgery can sometimes lead to bowel complications, including bowel perforation or obstruction.
- Bleeding: Ongoing bleeding or discharge from the vagina may occur as a result of transvaginal mesh surgery.
- Neuromuscular Alterations: Transvaginal mesh implants can potentially cause changes in the nerves and muscles of the pelvic region, leading to altered sensation or function.
- Lower Urinary Tract Symptoms (LUTS): LUTS, such as urinary frequency, urgency, or incontinence, can be experienced by some women after transvaginal mesh surgery.
- Vaginal Scarring: Scarring of the vaginal tissue can occur as a result of transvaginal mesh surgery.
- Immune Disorders: In rare cases, transvaginal mesh implants have been associated with immune disorders.
It is important to discuss these potential complications with your healthcare provider and weigh the risks and benefits before undergoing transvaginal mesh surgery.
Table of Contents
What Are Common Transvaginal Mesh Complications?
Transvaginal mesh complications are increasingly becoming a concern among women who have undergone procedures using this surgical device.
These issues range from minor discomfort to severe pain and can significantly impact quality of life.
Common transvaginal mesh complications reported by women:
- Mesh erosion: where the material wears through the vaginal wall or surrounding tissues.
- Dyspareunia: pelvic pain which may be persistent or intermittent during intercourse.
- Bowel problems: like constipation, fecal incontinence or obstruction due to displacement of the intestine.
- Urinary issues: such as frequent infections, voiding dysfunction and incomplete bladder emptying.
Additionally, there’s an increased probability of bleeding both during and after surgery.
The risk extends further with potential damage to nerves within the surgical area leading to numbness or extreme sensitivity.
In spite of these known risks, transvaginal mesh continues to be utilized primarily due its high success rate in treating POP and SUI when compared with native tissue repair techniques alone.
Understanding Transvaginal Mesh
Transvaginal mesh is a type of surgical mesh, which acts like a net.
Transvaginal Mesh Usage
Doctors insert this medical device into women through the vagina during surgical procedures to repair damaged or weakened tissue in the pelvic area or bladder.
The concept behind this invention is that it provides additional support to muscles and ligaments that have become weak due to conditions such as childbirth, age, or obesity.
The application and functionality of transvaginal mesh vary depending on the needs of an individual patient.
Primarily crafted from synthetic materials such as polypropylene, these meshes can also be composed biologically from animal tissues.
It’s important to note that while these devices are designed for repairing issues related to urinary incontinence and pelvic organ prolapse (POP), their usage has raised significant concerns because of associated complications leading often to serious health risks.
Purpose and Functionality
Transvaginal mesh serves a crucial role in providing extra support to weakened or damaged tissues in the female pelvic area.
This synthetic or biological material is often utilized for treating conditions like pelvic organ prolapse and stress urinary incontinence where the body’s own structures fall short.
The mesh, once implanted through an invasive procedure, works as a scaffold allowing the body’s tissues to grow into it and strengthen over time.
While effective, transvaginal mesh complications can occur; understanding its function and purpose aids both patients and physicians in managing expectations from this medical solution.
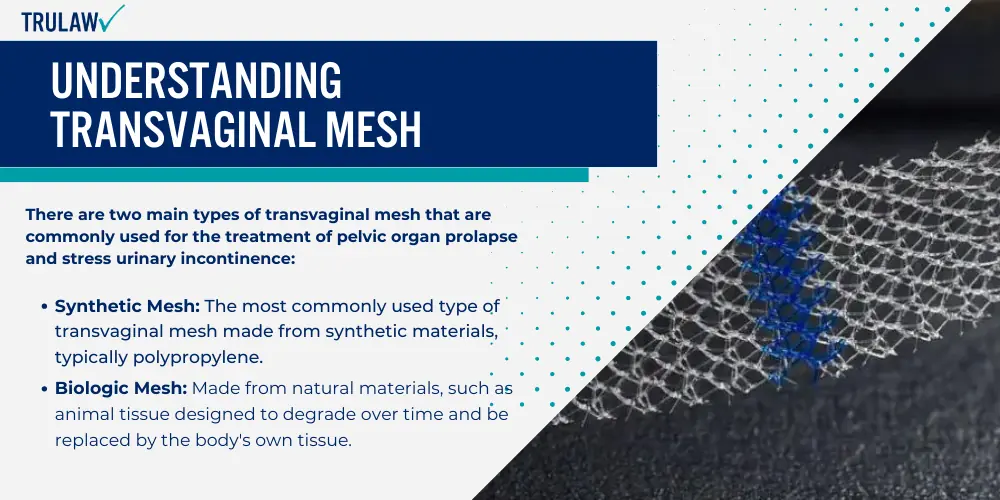
Types of Transvaginal Mesh
There are two main types of transvaginal mesh that are commonly used for the treatment of pelvic organ prolapse and stress urinary incontinence:
- Synthetic Mesh: The most commonly used type of transvaginal mesh made from synthetic materials, typically polypropylene, causing complications such as mesh erosion and infection.
- Biologic Mesh: Made from natural materials, such as animal tissue designed to degrade over time and be replaced by the body’s own tissue.
This makes it less durable than synthetic mesh, but it is also less likely to cause complications.
When deciding between these two types of mesh, it is important to consider factors such as the patient’s overall health, the severity of their condition, and their personal preferences.
It is also crucial to be aware of the potential complications and risks associated with each type of mesh.
Synthetic Mesh
Manufacturers construct synthetic mesh from a variety of materials, including polypropylene.
It is frequently used in transvaginal procedures to treat conditions like pelvic organ prolapse and stress urinary incontinence.
Even though it tends to provide lasting results due to its durability, complications may still occur.
The most common issue associated with synthetic mesh is erosion or extrusion into the vaginal tissue.
This complication has led the Food and Drug Administration (FDA) to state that problems resulting from these devices aren’t rare.
Another potential problem could be chronic pain experienced by patients after surgery involving synthetic mesh implantation.
Regardless of its benefits, doctors have stressed on the importance of analyzing both risks and advantages before deciding whether surgical use of synthetic mesh would be appropriate for each individual case.
Biologic Mesh
Biologic mesh is one type of transvaginal mesh that has a central role in the realm of pelvic reconstructive surgery.
This mesh, made from human or animal tissues, serves as a viable option when synthetic meshes are not desired or feasible.
Biologic mesh tends to integrate smoothly into the body, reducing certain complications like erosion and infection frequently associated with synthetic counterparts.
However, it’s important to note that while biologic mesh may have fewer immediate adverse effects compared to synthetic materials, it doesn’t mean they’re completely risk-free.
Even though these meshes are designed for better assimilation into the body’s structure, some patients might experience problems such as bladder outlet obstruction or voiding dysfunction post-surgery.
Therefore, understanding potential risks before any surgical procedure involving this kind of product plays an essential part in informed decision-making.
Common Uses of Transvaginal Mesh
Transvaginal mesh serves a critical role in the treatment of pelvic organ prolapse.
This medical condition, often seen in women post-childbirth or after menopause, occurs when the muscles and tissues supporting the pelvic organs weaken, causing these organs to drop (prolapse) into the vagina.
Treatment for Pelvic Organ Prolapse
To alleviate this issue, surgeons use transvaginal mesh — a net-like implant made from synthetic material or biologic tissue that provides additional support to weakened pelvic tissues and helps uphold displaced pelvic organs.
Pelvic reconstructive surgery involving transvaginal mesh can significantly improve patients’ quality of life by relieving discomfort associated with prolapse and restoring normal function.
However, it’s crucial for potential candidates to be aware of the possible complications linked with transvaginal mesh, such as mesh erosion and infection.
Management of Stress Urinary Incontinence
The use of transvaginal mesh for the management of stress urinary incontinence is a prevalent medical practice.
Transvaginal mesh provides support to weakened pelvic muscles, aiding in alleviating symptoms associated with this condition.
However, complications may arise, such as mesh erosion and pain.
Prompt diagnosis and treatment are essential to mitigate these issues.
Various strategies can be adopted for managing these complications–ranging from medications to surgical procedures like mesh revision or excision surgery.
Visiting your doctor regularly ensures early detection of any potential problems, while seeking guidance from a multidisciplinary team increases chances of better health outcomes.
Common Procedures Using Transvaginal Mesh
Several procedures commonly utilize Transvaginal Mesh to treat different health conditions:
- Midurethral Sling Procedure: This is the most common procedure that employs transvaginal mesh. It helps women manage stress urinary incontinence by providing support to the urethra.
- Anterior and Posterior Vaginal Wall Repair: In these surgeries, doctors use transvaginal mesh to fortify weakened vaginal walls that have resulted from pelvic organ prolapse.
- Sacrocolpopexy: This is a form of abdominal surgery where surgeons attach a piece of synthetic mesh around the top part of the vagina and secure it to the sacrum bone, preventing pelvic organ prolapse.
- Transobturator Tape Procedure: Similar to the midurethral sling procedure, this operation uses synthetic mesh tape through an incision in your groin area. The primary goal is to help control stress urinary incontinence.
- Colporrhaphy: In this surgery, doctors implant a transvaginal mesh as a reinforcement material within the vaginal wall for treating anterior or posterior compartment prolapse.
Potential Complications Associated with Transvaginal Mesh
This section explores the potential complications associated with transvaginal mesh, covering issues such as mesh erosion and infection, painful intercourse (dyspareunia), bowel complications, and pelvic pain.

Mesh Erosion
Mesh erosion is a severe complication related to transvaginal mesh surgery.
It occurs when the implanted mesh begins to wear away or tear, causing it to protrude into the nearby tissues and organs.
This issue might lead to other complications such as pain during sexual intercourse, multiple infections or even damage to surrounding structures like bladder or rectum.
The FDA has identified this problem as one of the most common post-surgical issues associated with transvaginal meshes.
Due to its seriousness, treating mesh erosion often requires another surgical intervention for either removal or revision of the eroded mesh piece.
Mesh Infection
Mesh infection is among the many complications associated with transvaginal mesh.
This issue often arises from contamination of the device during its insertion through a non-sterile passage, such as the vagina.
Infection signs linked to mesh complications may include various vaginal problems and wound issues like granulation tissue and sinus development.
Additionally, severe cases of mesh erosion into the bowel have been recorded as a complication related to this type of procedure, heightening concerns about potential infections.
Quick diagnosis and treatment are essential in managing these consequences effectively.
Mesh Retraction
Mesh retraction is a well-known complication associated with the use of transvaginal mesh in surgical procedures.
This problem occurs when the mesh begins to shrink, causing it to pull away from where it was initially placed.
As a result, patients may experience discomfort and symptoms that often lead them back to their healthcare provider for evaluation.
The effects of mesh retraction can drastically impact quality of life.
It can lead to pelvic pain, irregular bleeding or even dyspareunia (pain during intercourse).
While some women notice these issues right after surgery, others might not until years later.
In fact, bladder sling complications can occur long after initial surgery according to an important study on this topic.
Dyspareunia (Painful Intercourse)
Dyspareunia, or painful intercourse, is a significant complication of transvaginal mesh surgery: It’s common for women to experience discomfort during sexual activities following the procedure.
This pain can be due to several factors including vaginal mesh extrusion and pelvic pain associated with the surgical treatment.
Research indicates that dyspareunia is more likely to occur after transvaginal procedures for pelvic organ prolapse repair using mesh than in abdominal surgeries.
The frequency or prevalence of this uncomfortable condition as a complication from transvaginal meshes isn’t specifically noted in clinical studies, yet it remains an important concern among patients and healthcare providers alike.
Treatment strategies often focus on managing other complications such as mesh erosion, which may contribute to the development of dyspareunia.
Bowel Complications
Transvaginal mesh can sometimes erode into the bowel, leading to complications.
This condition is marked by troubling symptoms such as abdominal pain and changes in bowel movements.
While this isn’t a common occurrence, it’s crucial to acknowledge its possibility when assessing the potential risks associated with transvaginal mesh procedures.
Medical practitioners need to stay vigilant while monitoring patients who’ve undergone such surgeries for any signs of these issues.
Pelvic Pain
Pelvic pain stands as a primary concern in transvaginal mesh complications.
This discomfort occurs when the implanted mesh triggers adverse reactions, causing sensitivity and agony within the pelvic region.
Due to the mesh’s close proximity to various internal organs, inflicted discomfort can be significant and impact an individual’s daily life substantially.
Notably, this pelvic pain may also extend to sexual intercourse, medically referred as dyspareunia.
Being persistent or intermittent, such pain might necessitate further medical intervention, like surgical removal of the invasive mesh.
In some instances, despite not being externally visible or exposed, internal irritation by nonexposed mesh still significantly contributes to enduring pelvic distress.
Given these circumstances, effective management strategies for coping with excruciating pelvic suffering are integral parts of treating complications associated with transvaginal meshes.
Incidence and Risk Factors
Incidence of Complications
Transvaginal mesh complications occur more frequently than expected, making it a serious concern for patients undergoing pelvic organ prolapse repair or stress urinary incontinence treatments.

Studies indicate that mesh-related problems are not unusual as they can appear after any type of midurethral sling placement such as:
- Retropubic;
- Transobturator; and
- Single incision techniques.
The most common issues include erosion through vaginal epithelium, infection, pain, urinary problems, recurrence of prolapse and/or incontinence.
Furthermore, evidence suggests the incidence rates for specific complications like mesh exposure (extrusion/erosion) and pain are quite high in individuals who have undergone pelvic floor reconstructive surgery using tapes or slings.
Hemorrhage, organ perforation alongside other symptoms like infection could also emerge following a stress urinary incontinence procedure with surgical mesh devices.
Hence these trends highlight the urgent need to adopt safer practices when dealing with transvaginal meshes.
Risk Factors for Complications
Certain lifestyle choices and health conditions can increase the likelihood of complications from transvaginal mesh.
For instance, obesity poses a significant risk due to increased intra-abdominal pressure that can strain the pelvic floor muscles and compromise healing post-surgery.
This additional strain may result in complications such as mesh erosion or infection.
In addition, poorly controlled diabetes is another noteworthy risk factor.
High blood sugar levels can slow down the body’s healing process after surgery, increasing susceptibility to infections, thereby leading to severe complications like urinary problems or chronic pelvic pain.
Moreover, smoking and tobacco use have been associated with delayed wound healing and higher rates of surgical infections.
These habits could endanger patients undergoing transvaginal mesh procedures by exacerbating risks like vaginal bleeding or incomplete bladder emptying following surgery.
Diagnosis and Assessment of Mesh Complications
Doctors employ several methods to diagnose and assess transvaginal mesh complications.
A detailed medical history paired with a thorough physical examination forms the basis of diagnosing mesh-related issues.
Erosions through the vaginal epithelium, infection, pain, urinary problems are key symptoms that suggest possible mesh complications.
An increased understanding of these symptoms can lead to early diagnosis and timely management.
Specialists use specific diagnostic tests for assessing whether surgical mesh is causing complications.
Imaging techniques like ultrasound and MRI help visualize the placement of transvaginal mesh in the body.
Sequential examinations may also be necessary to monitor any changes over time or response to treatments provided.
To accurately classify and standardize patient experiences with transvaginal mesh issues, a multidisciplinary team approach often proves valuable.
This collaborative process enables specialists across various fields like urology, gynecology, physiotherapy among others to contribute their insights into forming an accurate diagnosis leading to personalized treatment plans.
The potential severity of complications associated with surgical meshes such as painful intercourse or bowel complications requires a meticulous assessment process in order to ensure effective treatment options are identified promptly for affected patients.
Diagnostic Tests
A critical part of managing transvaginal mesh complications is through Diagnostic Tests, which include:
Classification and Standardization
The classification and standardization of transvaginal mesh complications are essential components in the diagnosis and treatment process.
This system helps healthcare professionals to accurately categorize ailments, leading to a more effective management strategy for each individual patient.
The standardized terminology used in diagnosing mesh complications aids seamless communication among multidisciplinary teams involved in patient care.
Similarly, descriptions of surgical procedures have also been uniformed for better understanding and execution across medical practice.
Notably, the classification system for transvaginal mesh used in pelvic organ prolapse repair is considered one of the riskiest medical devices due to its potential complications.
Therefore, adherence to these standards greatly contributes to patients’ safety while ensuring consistent quality care across different healthcare settings.
Diagnostic Pathways
Physicians often use various diagnostic pathways to identify transvaginal mesh complications:
- Physical Examination: This process involves a thorough evaluation of the patient. The doctor might check for any noticeable abnormalities, such as mesh erosion.
- Urine Analysis: This lab test helps determine if there are any signs of infection or other urinary abnormalities.
- Urodynamic Studies: These studies evaluate how well the bladder, sphincters, and urethra are performing their job of storing and releasing urine.
- Cystoscopy: This diagnostic procedure allows the doctor to visually examine the interior of a woman’s bladder and urethra.
- Imaging Studies: Techniques like X-rays, CT scans, MRI scans and ultrasound can be utilized to visualize internal structures and assess the position of the mesh implant.
- Patient History Assessment: Doctors may listen to descriptions of symptoms, previous surgeries or procedures that could have contributed to current issues.
Multidisciplinary Team Involvement
Multidisciplinary team involvement plays an essential role in handling transvaginal mesh complications.
Experts from various medical fields unite, sharing their unique knowledge to tackle these complex issues effectively.
Management of Transvaginal Mesh Complications
There are varying methods for the management of transvaginal mesh complications.
Each treatment approach is patient-specific, designed depending on the severity and type of complication.
For minor complications like small areas of exposed mesh, non-surgical treatments may be effective.
These could include estrogen cream application, antibiotics for infection control, or even ‘watchful waiting’ to monitor potential changes in symptoms.
In more severe cases where large portions of the mesh have eroded into surrounding organs, surgical intervention becomes necessary.
Surgery often includes removal or revision of part or all the offending mesh.
Despite this drastic measure, it’s important to remember that not all pain will disappear post-surgery because scar tissue from previous surgeries can contribute to chronic discomfort.
In such situations, multidisciplinary teams including urologists and pain management specialists become crucial in providing comprehensive care designed to minimize distress and improve quality of life.
Conservative Management

When it comes to the management of transvaginal mesh complications, several treatment options are available under conservative management:
Treatment Options
Transvaginal mesh complications may require one of the following (7) treatment options, such as:
- Observation: The initial step in managing any complication is to monitor the patient’s condition closely. Through regular check-ups and follow-up appointments, health care providers keep a watchful eye on any changes or developments.
- Physical Therapy: This therapeutic approach targets the muscles of the pelvic floor. By strengthening these muscles, physical therapy can often alleviate some of the discomfort associated with transvaginal mesh complications.
- Medication: Depending on the nature and severity of the complications, doctors may prescribe pain relievers, antibiotics for infection, or other medications to manage symptoms.
- Conservative Management: A non-invasive treatment approach includes managing symptoms with physical therapy and medication before considering surgical intervention.
- Surgical Intervention: In severe cases where conservative management is ineffective, surgical intervention may be necessary to remove or adjust the problematic mesh.
- Counseling or Support Services: Dealing with medical complications is not only physically challenging but also psychologically demanding. Mental health professionals can provide coping strategies and emotional support throughout the treatment journey.
- Ongoing Follow-up Care: Even after successful treatment of immediate complications, patients are advised to maintain regular follow-ups with their healthcare provider to ensure that there are no delayed adverse effects from their surgeries.
Mesh Revision: Excision Surgery
The goal of this surgical approach is to treat the problem caused by the mesh without causing additional damage or distress to patients.
Typically, surgeons perform these procedures laparoscopically – using small incisions instead of large ones employed in traditional surgeries.
This method decreases patient discomfort and promotes swift recovery after surgery while efficiently resolving issues related to the mesh.
Minimally invasive surgery stands as a preferred method for managing transvaginal mesh complications.
It reduces the potential risks and recovery time associated with open surgeries.
Interventions may involve procedures such as removal, revision, or repair of the mesh implant.
Patient Involvement in Management
Involving patients in the management of transvaginal mesh complications contributes to better treatment outcomes.
This patient-centered approach promotes open dialogue between healthcare providers and patients, enabling a mutual decision-making process.
Patients actively engage in discussing potential risks, benefits, alternatives to treatment options, and their preferences.
Strong communication skills can assist patients in expressing their concerns about complication symptoms or post-surgical discomfort more precisely and confidently.
Healthcare professionals then utilize these inputs to customize the therapeutic approach for each patient accordingly.
Further, educating patients on preventative measures reduces chances of recurrent complications related to transvaginal mesh procedures.
Moreover, equipping patients with knowledge about self-care instructions accelerates recovery time post-surgery and aids efficient long-term management of any possible issues associated with transvaginal mesh implants.
Empowering them with resources such as support groups or helpline services can also contribute significantly towards their mental well-being during this challenging period.
Multidisciplinary Approach
Understanding the multifaceted management of transvaginal mesh complications, there’s a need for a multidisciplinary approach involving healthcare professionals such as urologists, gynecologists, and physical therapists.
Legal Aspects: Understanding Transvaginal Mesh Lawsuits
The legality surrounding transvaginal mesh complications is heavily entwined with the lawsuits filed by patients who faced adverse effects post-surgery.
Hundreds of thousands of women have sought legal recourse, alleging severe pain, bleeding, organ perforation and other health issues stemming from this medical procedure.
These lawsuits argue that manufacturers failed to sufficiently warn patients about potential risks and side-effects of these devices.
Some cases have resulted in significant financial settlements – one being among the largest transvaginal mesh settlements till date!
The courtrooms stand as a battleground where affected individuals can fight for justice and recompense against considerable trauma they endured due to alleged negligence on part of product manufacturers.
In essence, understanding the legal aspects associated with this issue enables people to identify their rights should they too face any complications after undergoing a surgery involving transvaginal mesh.
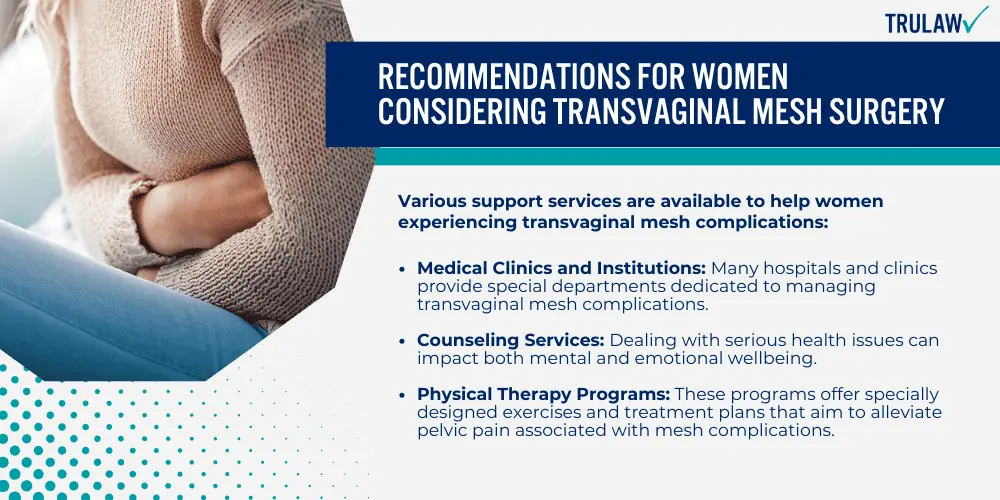
Recommendations for Women Considering Transvaginal Mesh Surgery
Before opting for transvaginal mesh surgery, it’s imperative to fully understand all aspects of the procedure, potential complications, and available alternative treatments.
Here are some recommendations that women should consider:
Seeking Medical Advice
If you’ve had transvaginal mesh surgery or are considering it, reaching out to medical professionals is crucial for understanding your health situation.
Your healthcare provider can explain the specific details of transvaginal mesh complications and answer any questions you may have about surgical procedures.
Regardless if symptoms appear immediately after the procedure or years later, contacting a physician promptly is essential in managing any potential issue effectively.
Healthcare providers offer guidance that can help navigate through decision-making processes, monitor healing progress post-surgery and address worries related to chronic pain.
Furthermore, psychologists can play a significant role by offering emotional support to women experiencing mesh complications; they channel vital resources to prepare patients for medical procedures and manage chronic pain more sustainably.
Support Services Available
Various support services are available to help women experiencing transvaginal mesh complications:
- Helplines and Hotlines: These services offer immediate assistance, information or resources over the phone. It’s a quick way to get in touch with medical experts who understand your situation or guide you through complex procedures.
- Medical Clinics and Institutions: Many hospitals and clinics provide special departments dedicated to managing transvaginal mesh complications. They have skilled professionals who can analyse your symptoms and propose suitable treatments.
- Online Support Groups: Connecting with others who face similar challenges allows for supportive interactions, shared experiences, and helpful advice.
- Counseling Services: Dealing with serious health issues can impact both mental and emotional wellbeing. Licensed therapists or counselors can equip patients to handle this stress more effectively.
- Legal Assistance: Law firms such as TruLaw specialize in cases relating to transvaginal mesh lawsuits, guiding victims through complex legal proceedings for claims against faulty implants.
- Physical Therapy Programs: These programs offer specially designed exercises and treatment plans that aim to alleviate pelvic pain associated with mesh complications.
- Patient Advocacy Organizations: Such institutions help by providing necessary education, advocating for patient rights, supporting research efforts, and promoting awareness about the associated risks of transvaginal meshes.
- Drug Counseling services: For those dealing with side effects from medication prescribed due to complications such as chronic pelvic pain or urinary issues, these experts assist in understanding drug interactions and managing medication intake effectively.
What to Do If You Are Experiencing Pain or Discomfort
Sudden pain or changes in bodily functions may mark early signs of complications, such as mesh erosion or organ perforation.
The healthcare provider will determine the best course of action based on symptoms and severity – this might include further diagnostic tests, a diverse range of treatments varying from conservative management to invasive surgeries like mesh revision/excision.
Never be hesitant to seek out help when you sense something is wrong.
Your health could vastly improve with timely intervention.
Seeking Help and Support
Those experiencing complications after a transvaginal mesh procedure should seek professional aid promptly.

The right support can lead to proper management of transvaginal mesh complications and improved quality of life.
Victorian Mesh Information and Helpline
The Victorian Mesh Information and Helpline exist as a valuable resource for those facing complications from transvaginal mesh surgeries.
Providing comfort, guidance, and answers to questions you may have, the helpline stands as an invaluable support line particularly focused on aiding individuals in the Victorian region of Australia.
They can direct you toward appropriate health professionals while offering educational materials aimed at furthering your understanding of this issue.
Not only does this service offer personal assistance, but it also contributes to wider advocacy work by raising awareness about these medical complications within broader society.
The Victorian Mesh Information and Helpline embodies their mission of helping patients navigate through their struggles with compassion, expertise, and real-time assistance.
Contact TruLaw for a free consultation
For any individual undergoing the turmoil of transvaginal mesh complications, TruLaw is a resource that offers relief.
They provide a free consultation to those who are dealing with these complications or have concerns about defective meshes.
By simply visiting their website, individuals can access a confidential chatbot that helps determine if they qualify for services offered by TruLaw.
This not only includes advice and support for those affected by common transvaginal mesh complications such as vaginal burning, serious scarring, or chronic pain but also consultations regarding compensation claims associated with hernia mesh repair surgery failures.
Essentially, TruLaw acts as an ally in seeking justice against faulty mesh product manufacturers.
Information and Helpline Services
TruLaw serves as a valuable information and helpline service for those dealing with transvaginal mesh complications.
This website provides a host of resources to guide individuals who experience discomforting symptoms such as vaginal burning, severe scarring, and chronic pain related to the use of transvaginal mesh.
TruLaw also provides crucial assistance in understanding the legal intricacies involved in navigating possible lawsuits against manufacturers responsible for these complications.
Important safety alerts were released by the Food and Drug Administration (FDA) in July 2011.
The FDA’s warning acknowledged that serious complications associated with surgical mesh implants for Pelvic Organ Prolapse (POP) repair are not uncommon, a fact underlined by numerous patient experiences documented on the site.
Conclusion
As we’ve discovered, transvaginal mesh complications are a significant concern.
Women who have undergone this procedure should be vigilant about any signs of discomfort or irregularities, such as consistent pelvic pain or urinary problems.
It’s important to understand the risks involved and to seek medical advice promptly if you experience potential symptoms of a complication.
Always make sure to discuss alternatives with your healthcare provider before making an informed decision on surgery involving transvaginal mesh.
Transvaginal Mesh Lawsuit Frequently Asked Questions
-
What are common transvaginal mesh complications?
If you are experiencing any symptoms or complications related to transvaginal mesh placement, it is essential to consult with a healthcare professional for proper evaluation and treatment.
Several of the common transvaginal mesh complications associated with the surgical devices include:
- Organ perforation: In rare cases, transvaginal mesh can cause perforation or puncture of nearby organs, such as the bladder or rectum.
- Urinary problems: Voiding dysfunction and recurrent urinary tract infections (UTIs) have been linked to transvaginal mesh placement.
- Bowel complications: Transvaginal mesh can sometimes erode into the bowel, leading to symptoms such as fecal incontinence, painful defecation, and rectal bleeding.
- Vaginal scarring: The presence of transvaginal mesh can lead to vaginal scarring, which can cause discomfort or pain.
-
Can the placement of transvaginal mesh kits lead to pelvic floor disorders?
Yes, the incorrect placement of Transvaginal Mesh Kits has been commonly reported in pelvic floor disorders, requiring management of the mesh.
However, these kits are still permitted for treating stress urinary incontinence in sling procedures.
Additional complications with Transvaginal Mesh Kits have been commonly reported, such as:
- Bleeding and infection are common complications associated with the use of transvaginal mesh kits.
- Erosion and nerve damage are other serious complications that can arise from the use of these kits.
- Organ perforation, pain, painful sexual intercourse, vaginal scarring, and vaginal shrinkage are also possible complications.
-
What are the surgical treatment options for pelvic organ prolapse?
It is important to note that the choice of surgical treatment options will depend on various factors
The surgical treatment options for pelvic organ prolapse include:
- Sacrocolpopexy: This surgery involves attaching the vaginal vault to the sacrum using surgical mesh.
- Sacrohysteropexy: This surgery is used to repair uterine prolapse by attaching the cervix to the sacrum using surgical mesh.
-
What are the non-surgical treatment options for pelvic organ prolapse?
It is important to note that the choice of non-surgical treatment options will depend on various factors
Non-surgical treatment options for pelvic organ prolapse include:
- Pelvic floor exercises;
- Pessary use;
- Estrogen therapy;
- Physical therapy;
- Other various lifestyle modifications.
Consulting with a Transvaginal Mesh Attorney at TruLaw can help determine the most suitable non-surgical treatment options for your specific case.
-
What are the common symptoms of stress urinary incontinence (SUI)?
The common symptoms of stress urinary incontinence (SUI) include the involuntary leakage of urine during physical activities that increase abdominal pressure, as mentioned earlier.
This can occur during:
- Coughing
- Sneezing
- Laughing
- Exercising
Individuals with SUI may also experience a frequent urge to urinate, a feeling of incomplete bladder emptying, and the need to wear pads or protective garments to manage the leakage.

Managing Attorney & Owner
With over 25 years of legal experience, Jessica Paluch-Hoerman is an Illinois lawyer, a CPA, and a mother of three. She spent the first decade of her career working as an international tax attorney at Deloitte.
In 2009, Jessie co-founded her own law firm with her husband – which has scaled to over 30 employees since its conception.
In 2016, Jessie founded TruLaw, which allows her to collaborate with attorneys and legal experts across the United States on a daily basis. This hypervaluable network of experts is what enables her to share the most reliable, accurate, and up-to-date legal information with our readers!
Additional Transvaginal Mesh Lawsuit resources on our website:
Here, at TruLaw, we’re committed to helping victims get the justice they deserve.
Alongside our partner law firms, we have successfully collected over $3 Billion in verdicts and settlements on behalf of injured individuals.
Would you like our help?
At TruLaw, we fiercely combat corporations that endanger individuals’ well-being. If you’ve suffered injuries and believe these well-funded entities should be held accountable, we’re here for you.
With TruLaw, you gain access to successful and seasoned lawyers who maximize your chances of success. Our lawyers invest in you—they do not receive a dime until your lawsuit reaches a successful resolution!
AFFF Lawsuit claims are being filed against manufacturers of aqueous film-forming foam (AFFF), commonly used in firefighting.
Claims allege that companies such as 3M, DuPont, and Tyco Fire Products failed to adequately warn users about the potential dangers of AFFF exposure — including increased risks of various cancers and diseases.
Depo Provera Lawsuit claims are being filed by individuals who allege they developed meningioma (a type of brain tumor) after receiving Depo-Provera birth control injections.
A 2024 study found that women using Depo-Provera for at least 1 year are five times more likely to develop meningioma brain tumors compared to those not using the drug.
Suboxone Tooth Decay Lawsuit claims are being filed against Indivior, the manufacturer of Suboxone, a medication used to treat opioid addiction.
Claims allege that Indivior failed to adequately warn users about the potential dangers of severe tooth decay and dental injuries associated with Suboxone’s sublingual film version.
Social Media Harm Lawsuits are being filed against social media companies for allegedly causing mental health issues in children and teens.
Claims allege that companies like Meta, Google, ByteDance, and Snap designed addictive platforms that led to anxiety, depression, and other mental health issues without adequately warning users or parents.
Transvaginal Mesh Lawsuits are being filed against manufacturers of transvaginal mesh products used to treat pelvic organ prolapse (POP) and stress urinary incontinence (SUI).
Claims allege that companies like Ethicon, C.R. Bard, and Boston Scientific failed to adequately warn about potential dangers — including erosion, pain, and infection.
Bair Hugger Warming Blanket Lawsuits involve claims against 3M — alleging their surgical warming blankets caused severe infections and complications (particularly in hip and knee replacement surgeries).
Plaintiffs claim 3M failed to warn about potential risks — despite knowing about increased risk of deep joint infections since 2011.
Baby Formula NEC Lawsuit claims are being filed against manufacturers of cow’s milk-based baby formula products.
Claims allege that companies like Abbott Laboratories (Similac) and Mead Johnson & Company (Enfamil) failed to warn about the increased risk of necrotizing enterocolitis (NEC) in premature infants.
Here, at TruLaw, we’re committed to helping victims get the justice they deserve.
Alongside our partner law firms, we have successfully collected over $3 Billion in verdicts and settlements on behalf of injured individuals.
Would you like our help?
