Transvaginal mesh is a piece of surgical netting that’s used to reinforce the vaginal wall and support pelvic organs in women dealing with pelvic floor disorders, most notably pelvic organ prolapse and stress urinary incontinence.
This synthetic or biologic mesh is designed from materials such as polypropylene or animal tissue, offering diverse options for patients based on their unique needs.
Definition and Purpose
The purpose of this mesh is to provide support and reinforcement for weakened or damaged tissue.
By bolstering the pelvic organs and vaginal wall, it helps reduce discomfort, improve functionality, and enhance quality of life for affected women.
Despite potential complications, experts deem careful positioning of the transvaginal mesh safe, while stating that its use often results in lower rates of repeat surgeries for prolapse compared to other treatments.
Types of Transvaginal Mesh
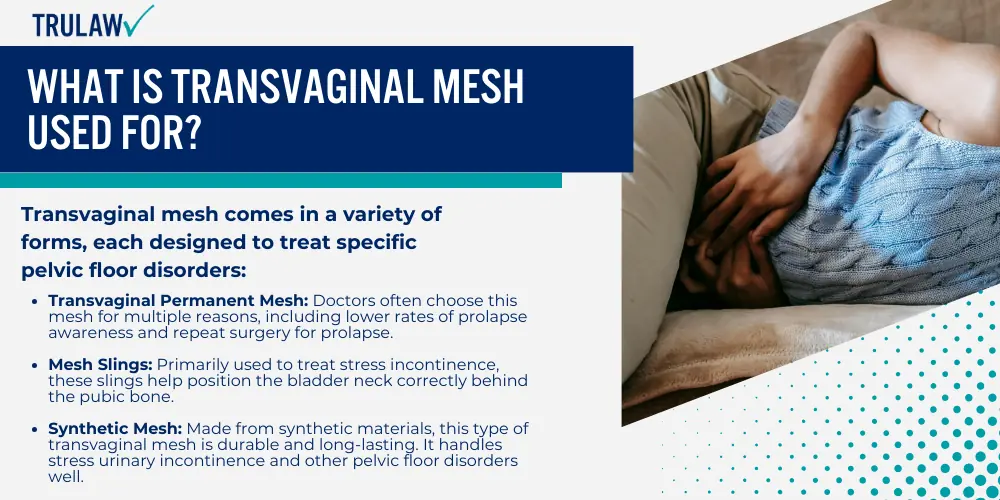
Transvaginal mesh comes in a variety of forms, each designed to treat specific pelvic floor disorders:
- Transvaginal Permanent Mesh: Doctors often choose this mesh for multiple reasons, including lower rates of prolapse awareness and repeat surgery for prolapse.
- Mesh Slings: Primarily used to treat stress incontinence, these slings help position the bladder neck correctly behind the pubic bone.
- Synthetic Mesh: Made from synthetic materials, this type of transvaginal mesh is durable and long-lasting. It handles stress urinary incontinence and other pelvic floor disorders well.
- Biologic Mesh: Biological mesh devices have received FDA approval based on their “substantial equivalence” to synthetic meshes, bypassing the standard clinical trial process. Studies on these devices have inconsistently reported clinical outcomes like infection rates.
- Type I Monofilament Mesh: This large-pore polypropylene mesh primarily aids in treating pelvic organ prolapse. It effectively offers support to weakened vaginal walls.