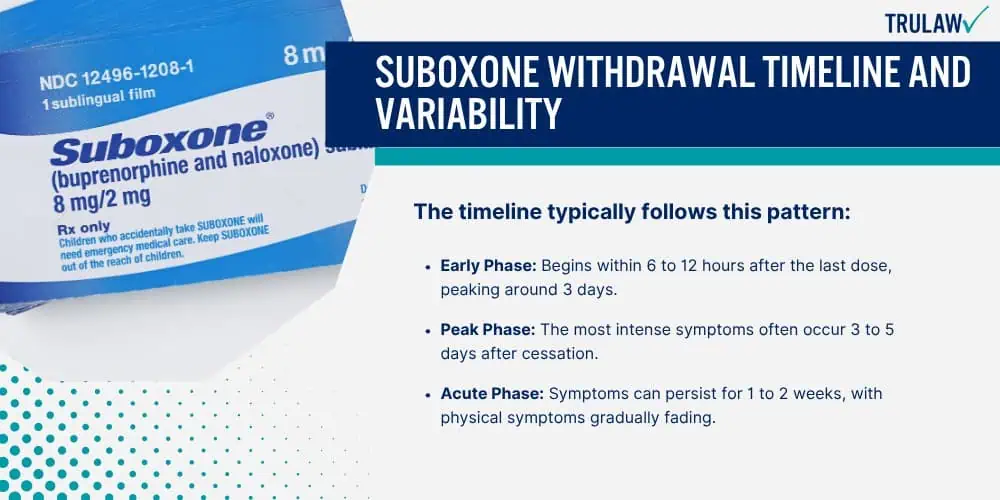
When a person stops taking Suboxone, a medication used to treat opioid dependence, they may experience a range of withdrawal symptoms.
These symptoms can vary in intensity and duration based on several factors.
Factors Influencing Suboxone Withdrawal Severity
Withdrawal from Suboxone can be influenced by various factors, making the experience fairly unique for each person.
Key considerations include:
- Duration of Use: The length of time someone has been taking Suboxone often correlates with the severity of withdrawal symptoms.
- Dosage: Higher doses of Suboxone can lead to more intense withdrawal symptoms when the medication is stopped or reduced.
- Individual Metabolism: Variations in a person’s metabolism can affect how quickly Suboxone is processed and eliminated from the body.
- Physical Health: Overall health can affect the intensity and duration of withdrawal symptoms.
- Psychological Factors: Mental health and personal stress levels can impact how severe withdrawal symptoms feel.
- Support systems: A strong support system can help alleviate the perception of withdrawal severity.
Withdrawal symptoms can include nausea, headaches, mood swings, and insomnia.
In cases where Suboxone is discontinued abruptly, symptoms may be more severe.
On the other hand, a gradual tapering of the medication, as part of a professionally supervised treatment plan, can often help to reduce the severity of withdrawal symptoms.