FDA Receives Reports Linking Type 2 Diabetes Drug With Serious Skin Diseases
- Last Updated: August 4th, 2023

Attorney Jessica Paluch-Hoerman, founder of TruLaw, has over 28 years of experience as a personal injury and mass tort attorney, and previously worked as an international tax attorney at Deloitte. Jessie collaborates with attorneys nationwide — enabling her to share reliable, up-to-date legal information with our readers.
Legally Reviewed
This article has been written and reviewed for legal accuracy and clarity by the team of writers and legal experts at TruLaw and is as accurate as possible. This content should not be taken as legal advice from an attorney. If you would like to learn more about our owner and experienced injury lawyer, Jessie Paluch, you can do so here.
Fact-Checked
TruLaw does everything possible to make sure the information in this article is up to date and accurate. If you need specific legal advice about your case, contact us by using the chat on the bottom of this page. This article should not be taken as advice from an attorney.
FDA Receives Reports Linking Type 2 Diabetes Drug With Serious Skin Diseases
The U.S. Food and Drug Administration (FDA) has received reports linking certain serious and painful skin diseases to Dipeptidyl peptidase (DPP-4) inhibitors, including:
- Bullous Pemphigoid
- Erythema multiforme
- Drug eruption
- Stevens-Johnson syndrome
- Eczema
- Oculomucocutaneous syndrome
The onset of these reactions typically occurred within the first three months of the initiation of treatment.
Sometimes they occur after the first dose.

Despite numerous reports of serious and painful skin diseases, the FDA has only required a label change to include the risk of Bullous Pemphigoid.
Each of the individuals reported having Bullous Pemphigoid resulted in a serious outcome, with half requiring hospitalization and one resulting in death, according to the FDA.
Table of Contents
Symptoms of Bullous Pemphigoid
Bullous Pemphigoid is a rare skin disorder that causes rashes and blistering.
Symptoms of the condition include:
- Blistering on the arms, legs, abdomen, and mucous membranes of the eyes, nose, mouth, and genitals.
- Red rash (develops before blistering).
- Large, fluid-filled blisters (usually clear, may contain blood).
- Skin around blisters appears normal, slightly red, or dark.
- Sensitive and painful ruptured blisters.
- Hives and itching.
A physician or dermatologist diagnoses Pemphigoid by performing a biopsy of the affected area.
What are DPP-4 Inhibitors and How Do They Work?
DPP-4 inhibitors are medications that, when used in combination with diet and exercise, can lower blood sugar in adults suffering from type 2 diabetes.
The FDA approved the first DPP-4 inhibitor, Januvia, in 2006.
DPP-4 inhibitors work in an entirely different way than other diabetes medications, which inhibit an enzyme in the gut that breaks down the hormones that help lower blood glucose.
DPP-4 inhibitors inactivate hormones called incretins in the gut, promoting higher levels of incretins to keep blood glucose in the normal range, particularly after meals.

Managing Attorney & Owner
With over 25 years of legal experience, Jessica Paluch-Hoerman is an Illinois lawyer, a CPA, and a mother of three. She spent the first decade of her career working as an international tax attorney at Deloitte.
In 2009, Jessie co-founded her own law firm with her husband – which has scaled to over 30 employees since its conception.
In 2016, Jessie founded TruLaw, which allows her to collaborate with attorneys and legal experts across the United States on a daily basis. This hypervaluable network of experts is what enables her to share the most reliable, accurate, and up-to-date legal information with our readers!
Here, at TruLaw, we’re committed to helping victims get the justice they deserve.
Alongside our partner law firms, we have successfully collected over $3 Billion in verdicts and settlements on behalf of injured individuals.
Would you like our help?
At TruLaw, we fiercely combat corporations that endanger individuals’ well-being. If you’ve suffered injuries and believe these well-funded entities should be held accountable, we’re here for you.
With TruLaw, you gain access to successful and seasoned lawyers who maximize your chances of success. Our lawyers invest in you—they do not receive a dime until your lawsuit reaches a successful resolution!
AFFF Lawsuit claims are being filed against manufacturers of aqueous film-forming foam (AFFF), commonly used in firefighting.
Claims allege that companies such as 3M, DuPont, and Tyco Fire Products failed to adequately warn users about the potential dangers of AFFF exposure — including increased risks of various cancers and diseases.
Depo Provera Lawsuit claims are being filed by individuals who allege they developed meningioma (a type of brain tumor) after receiving Depo-Provera birth control injections.
A 2024 study found that women using Depo-Provera for at least 1 year are five times more likely to develop meningioma brain tumors compared to those not using the drug.
Suboxone Tooth Decay Lawsuit claims are being filed against Indivior, the manufacturer of Suboxone, a medication used to treat opioid addiction.
Claims allege that Indivior failed to adequately warn users about the potential dangers of severe tooth decay and dental injuries associated with Suboxone’s sublingual film version.
Social Media Harm Lawsuits are being filed against social media companies for allegedly causing mental health issues in children and teens.
Claims allege that companies like Meta, Google, ByteDance, and Snap designed addictive platforms that led to anxiety, depression, and other mental health issues without adequately warning users or parents.
Transvaginal Mesh Lawsuits are being filed against manufacturers of transvaginal mesh products used to treat pelvic organ prolapse (POP) and stress urinary incontinence (SUI).
Claims allege that companies like Ethicon, C.R. Bard, and Boston Scientific failed to adequately warn about potential dangers — including erosion, pain, and infection.
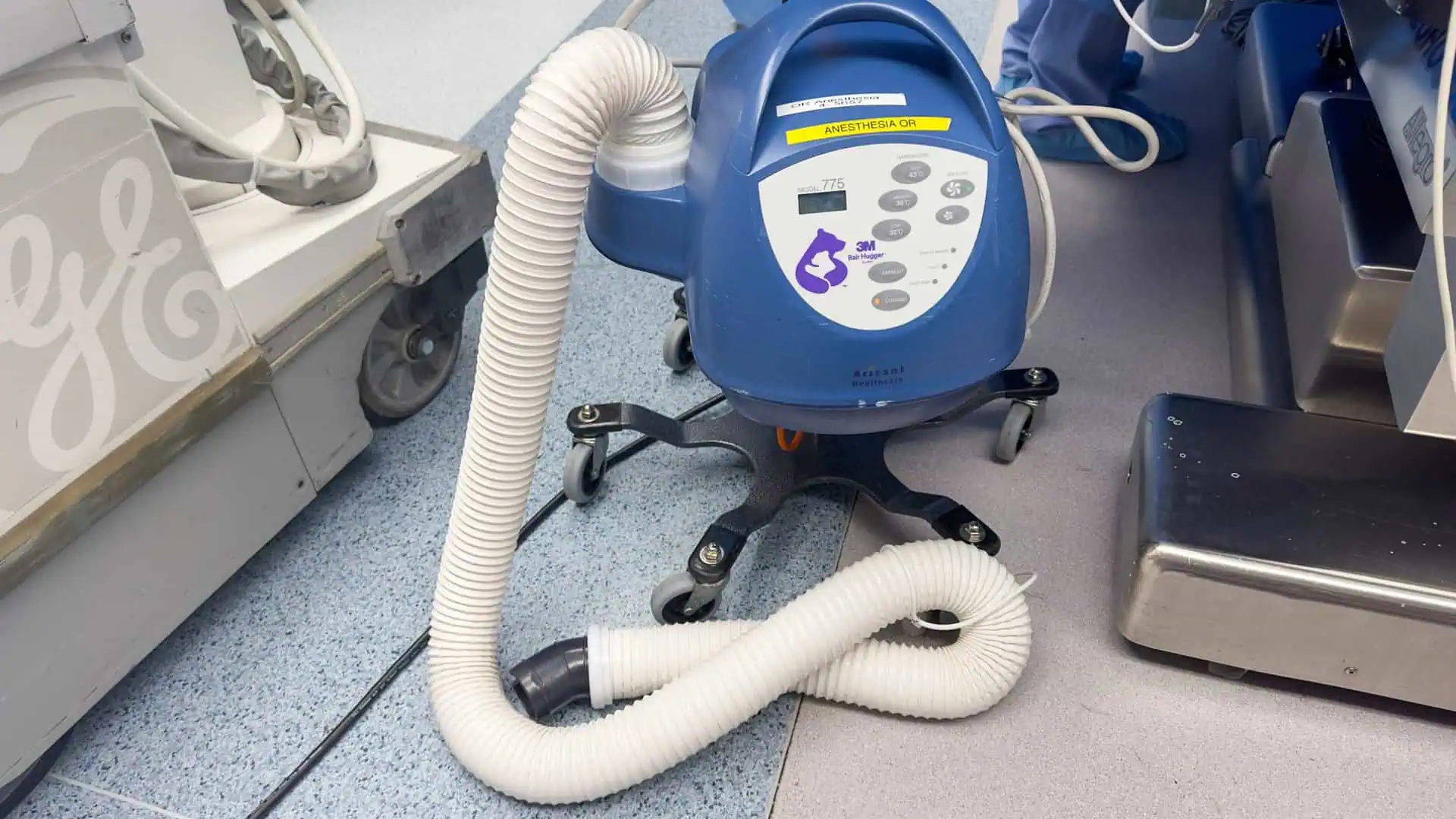
Bair Hugger Warming Blanket Lawsuits involve claims against 3M — alleging their surgical warming blankets caused severe infections and complications (particularly in hip and knee replacement surgeries).
Plaintiffs claim 3M failed to warn about potential risks — despite knowing about increased risk of deep joint infections since 2011.
Baby Formula NEC Lawsuit claims are being filed against manufacturers of cow’s milk-based baby formula products.
Claims allege that companies like Abbott Laboratories (Similac) and Mead Johnson & Company (Enfamil) failed to warn about the increased risk of necrotizing enterocolitis (NEC) in premature infants.
Here, at TruLaw, we’re committed to helping victims get the justice they deserve.
Alongside our partner law firms, we have successfully collected over $3 Billion in verdicts and settlements on behalf of injured individuals.
Would you like our help?